Quiz
Multiple Meningiomas can be associated with which of the following genetic mutation?
- Mutation in NF1 gene located on the long arm of chromosome 21
- Mutation in NF2 gene located on the long arm of chromosome 22
- Mutation in NF1 gene located on the short arm of chromosome 21
- Mutation in NF2 gene located on the short arm of chromosome 22
Pathophysiology
Grossly, there are 2 configurations
| Globose meningioma | En plaque meningioma |
| Well defined dural mass | Dural thickening |
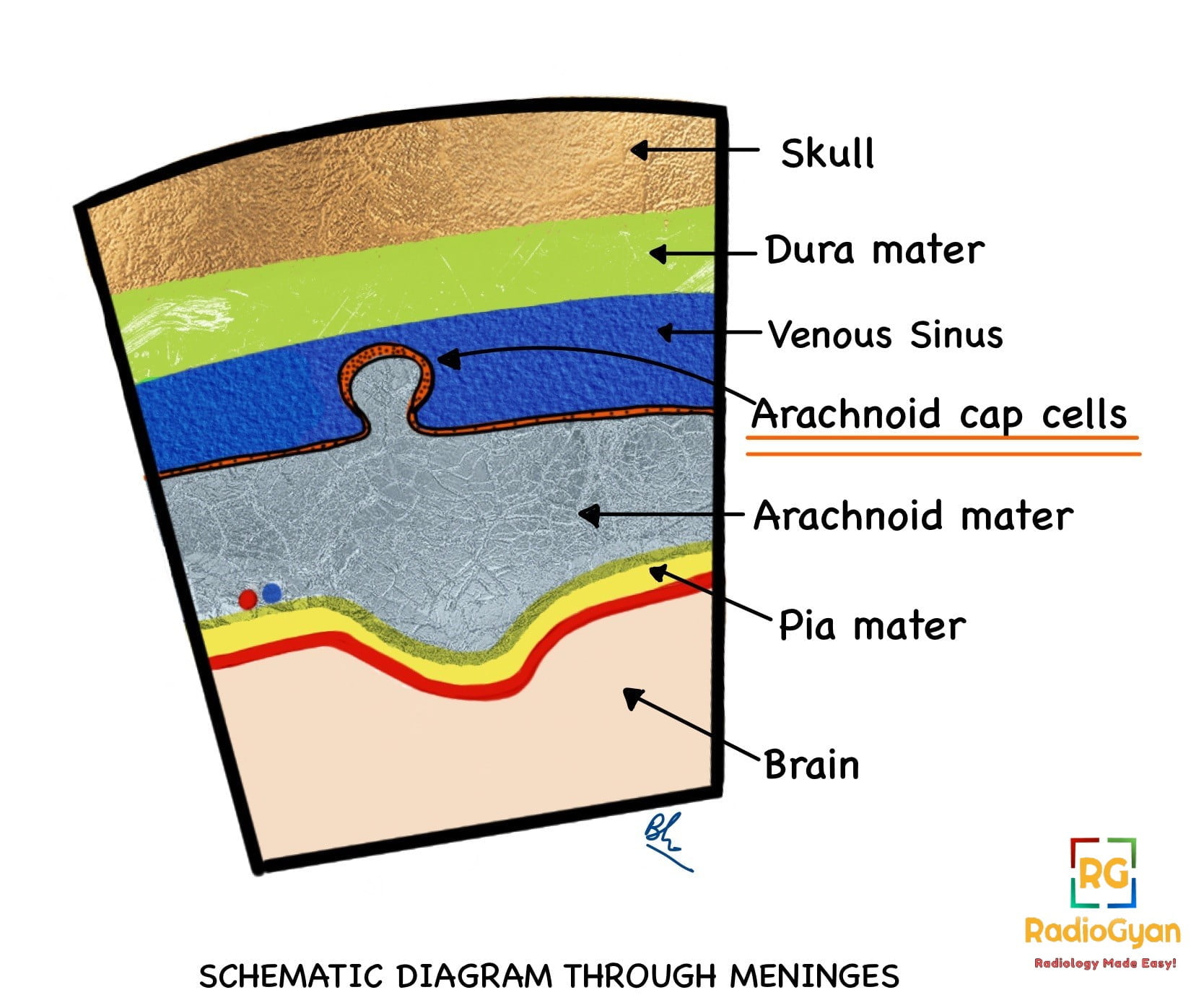
Meningioma arises from progenitor cells that give rise to arachnoid meningothelial (cap) cells situated outside the thin arachnoid layer that covers the brain and spinal cord.
Number:
Solitary in 90 % cases.
Multiple meningiomas are seen in :
- Neurofibromatosis 2
- Multiple Meningiomatosis syndrome
Location:
- Most common: Parasagittal > Convexity>Sphenoid ridge.
- Less common: Posterior fossa, olfactory groove, parasellar.
- Rare: Pineal, intraventricular, extracranial, intraosseous.
Skull Base Meningiomas: Meningiomas at the skull base can extend through the foramina, into the orbit and along the course of the trigeminal nerve.


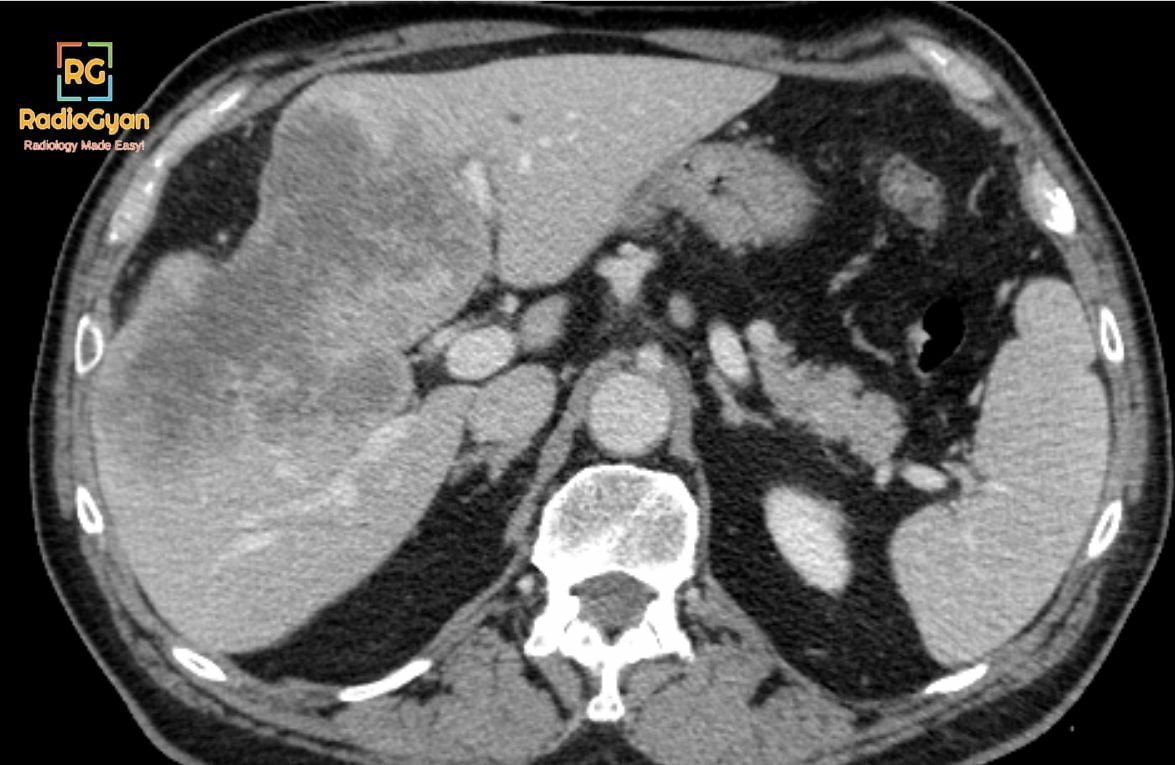
Key Imaging Features of typical lesions:
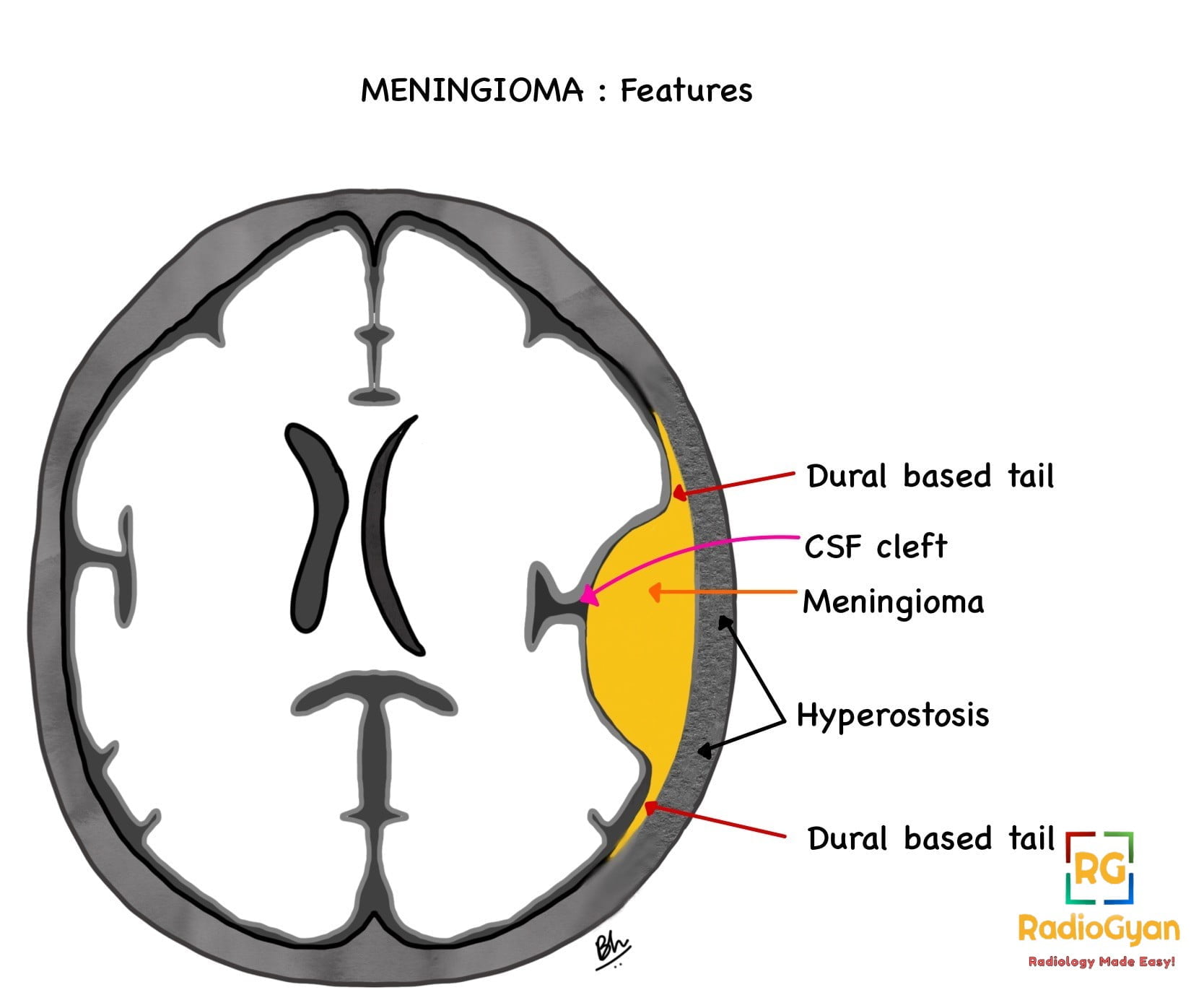
Meningiomas present as an extra-axial, lobular, well-circumscribed tumor with a broad-based dural attachment.

MRI:
- T1- Isointense to slight hypointense signal to grey matter.
- T2- Isointense to slight hyperintense signal to grey matter.
- FLAIR- Peritumoral edema is seen as a hyperintense signal in the adjacent brain parenchyma and is related to the presence of pial blood supply and VEGF expression and not to the tumour size or grade.
- T2* (GRE/SWI)- Intratumoral calcification.
- Post-contrast- Avid, homogeneous enhancement.
- Dural tail sign- Thickening and enhancement of the dura infiltrating away from the tumour.
- Sunburst pattern/ Spoke Wheel sign on MRI – Dural vascular supply seen as radiating vessels
- MR spectroscopy: Increased alanine, choline and decreased creatine.
- Features of extra-axial tumor- Buckling of the cortex,presence of a CSF cleft which is seen as T2 hyperintense rim between the tumour and the brain. and contains flow voids representing displaced vessels.
This CSF cleft sign if lost should raise suspicion of invasion of brain parenchyma.
- Signs of mass effect- Obstruction of CSF pathways, acquired intracranial herniation.
CT-
- The tumour appears mild to moderately hyperdense compared to a normal brain showing homogenous post-contrast enhancement. Calcifications within the tumor are better depicted on CT scans. Perilesional vasogenic edema is seen as hypodensity in the adjacent brain parenchyma.
- Bony changes– Hyperostosis is commonly seen in tumours arising from the skull base and anterior cranial fossa. The pathological causes of hyperostosis include direct tumour invasion of bone and reactive hypervascularity of the periosteum leading to benign bone formation. Bone lysis and destruction can also occur. Enlargement of the skull base foramina and adjacent paranasal sinuses occurs with skull base meningiomas.
Angiography/ DSA-
Meningioma has a dual blood supply, pial and dural.
‘Sunburst sign/ Spoke wheel sign’- dural vessels supply the centre of the lesion radiating toward the periphery. Pial vessels from the internal carotid artery supply the periphery of the tumour. Another angiographic sign is the mother-in-law sign- a prolonged vascular blush that persists late into the venous phase.

Radiographs are no longer used in the diagnosis of meningioma and the plain radiographic findings include erosion or hyperostosis of the bone, diffuse bony thickening, enlargement of the meningeal artery channel and calcification
Imaging Recommendation:
Contrast-enhanced MRI
Top 3 Differential Diagnosis:
- Haemangiopericytoma / solitary fibrous tumour of the dura- The lesion does not cause hyperostosis of the adjacent calvarium but can cause direct skull erosion. Tumours demonstrate heterogeneous enhancement, and prominent internal flow voids and may have a narrow, stalk-like or broad dural attachment
- Dural metastases- T2 hyperintense lesions with enhancing dural tail usually multiple in number and result from breast carcinoma, adenocarcinomas, squamous cell carcinoma of the lung and renal cell carcinoma.
- Primary dural lymphoma- Tumour shows T1 hypointense and T2 iso to hypointense signal compared to grey matter with vivid post-contrast enhancement and restricted diffusion on DWI.
Clinical Features:
- Symptoms– Usually asymptomatic. Symptoms depend on the size and location and occur due to the compression of the adjacent structures, including headache, seizure, visual field defect, cranial nerve palsies, hemiparesis and obstructive hydrocephalus.
- Age/Sex predilection– Female predilection, presenting in the 6th decade (mean age 65 years.)
- Risk factors– The majority of meningiomas are spontaneous. Risk factors include previous radiation exposure, genetic disorders such as neurofibromatosis type 2 and multiple meningiomatosis syndrome.
- Malunion causing dinner fork deformity
- Median nerve palsy
- Post-traumatic carpal tunnel syndrome
- Secondary osteoarthritis is frequently seen in intra-articular involvement.
- Extensor pollicis longus- tendon tear
Classification System :
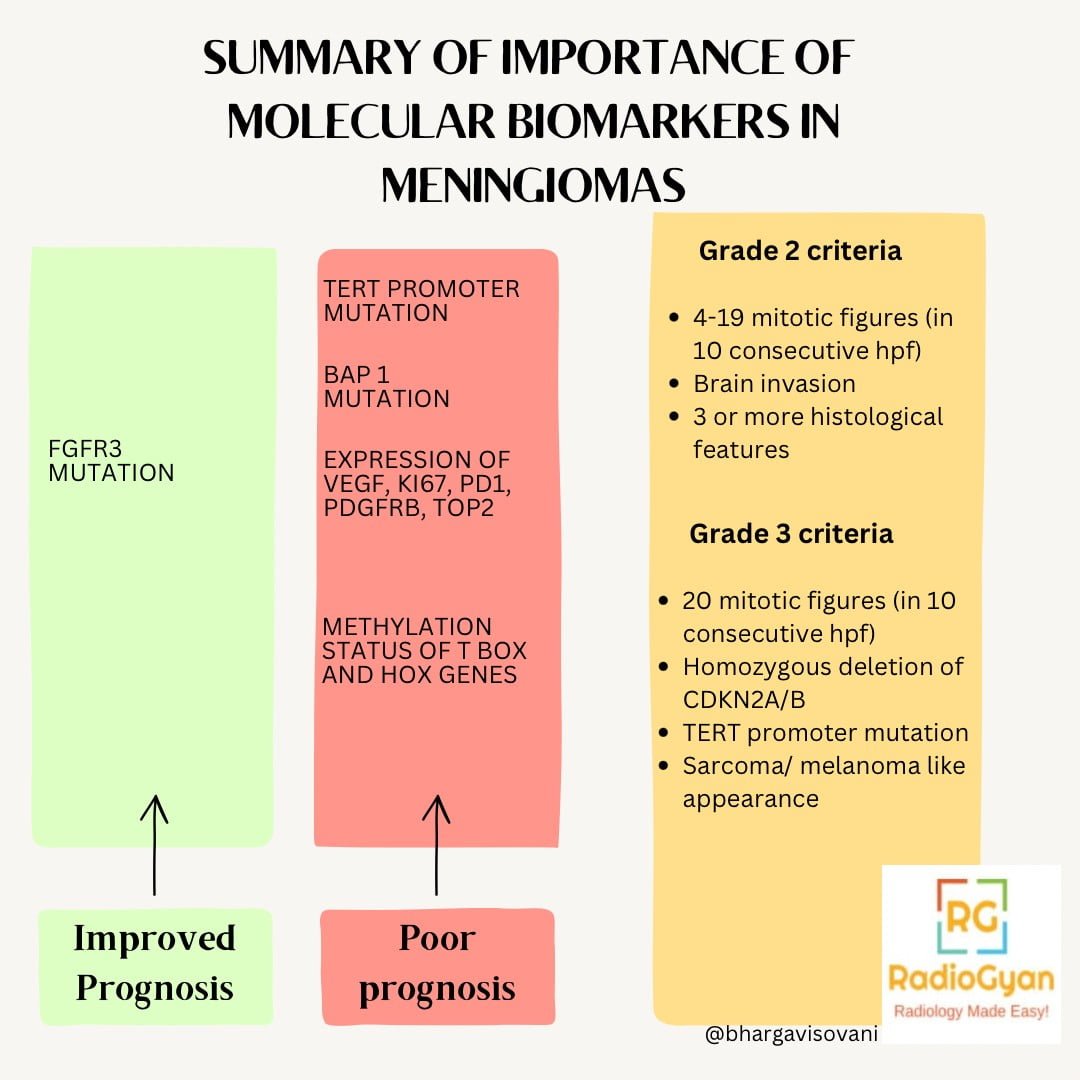
As per the 2021 WHO Classification of CNS tumours (5th edition) Meningioma is considered a single ‘type’, and its broad morphological spectrum is recognised as 15 ‘subtypes’.
Changes in the 5th edition of WHO classification of CNS tumours :
- Papillary meningioma, rhabdoid meningioma are no longer attributed to be high grade only based on the histology.
- Imaging features suggestive of brain invasion (except overt invasion) irrespective of histology is not assigned a grade 2 classification as was previously followed. This is because it may represent growth in perivascular planes, and not true invasion of brain parenchyma.
Histologically, the WHO grades meningioma into three categories-
Grade I – Most common type, benign lesions with non-aggressive growth and low recurrence risk. eg- meningothelial, fibroid, transitional, psammomatous, microcystic, secretory and angiomatous.
Grade II– ‘Atypical meningiomas’ – more aggressive clinical behaviour and less favourable outcome. eg- choroid and clear cell meningioma.
Grade III– Most aggressive form- ‘Anaplastic (malignant) meningiomas’, and usually papillary and rhabdoid.
Etymology and synonyms:
The term “meningioma” was used first by Harvey Cushing, an American neurosurgeon, to describe a set of tumors that occur in the brain and spinal cord, having various common features.
Treatment:
- Surgical resection using image guidance if lesion is symptomatic.
- ‘Simpson grading’ was used to define the extent of resection previously. However, owing to its subjective nature, and availability of more objective criteria to assess level of resection, like post operative MRI and 68-Ga DOTATATE PET, Simson grading is not used now.
- Meningioma in critical locations like cavernous sinus can be treated with stereotactic radiosurgery or chemotherapy with progesterone antagonist.
References:
Single best review article:
Other references:
- Osborn’s Brain: Imaging, Pathology, and Anatomy by Anne G. Osborn MD FACR (Author), Gary L. Hedlund DO (Author), Karen L. Salzman MD (Author)-Elsevier publication– 2nd edition. ISBN-10 : 9780323477765
- Siegelman ES, Mishkin MM, Taveras JM. Past, present, and future of radiology of meningioma. Radiographics. 1991;11(5):899-910. doi:10.1148/radiographics.11.5.1947324
- Louis DN, Perry A, Wesseling P, et al. The 2021 WHO Classification of Tumors of the Central Nervous System: a summary. Neuro Oncol. 2021;23(8):1231-1251. doi:10.1093/neuonc/noab106
- Al-Rashed, M., Foshay, K. and Abedalthagafi, M. (2020) ‘Recent advances in meningioma immunogenetics’, Frontiers in Oncology, 9. doi:10.3389/fonc.2019.01472.
Case co-authored by TeamGyan Members Dr Mansi Sarmalkar, Dr. Bhargavi Sovani