Quiz
Lhermitte Duclos disease is closely associated with which syndrome?
- Lynch syndrome
- Peutz Jeghers syndrome
- Familial Adenomatous Polyposis
- Cowden syndrome
Pathophysiology
Lhermitte Duclos disease is another name of dysplastic gangliocytoma of the cerebellum. There are different hypotheses regarding the lesion being neoplastic, vs. hamartomatous, vs. malformative. Grossly the lesion has a gyriform appearance. In this section, you’ll find a brief explanation of the histological changes related to the disease. Understanding these changes will help you grasp why the disease is known by different names, as explained in the etymology section.
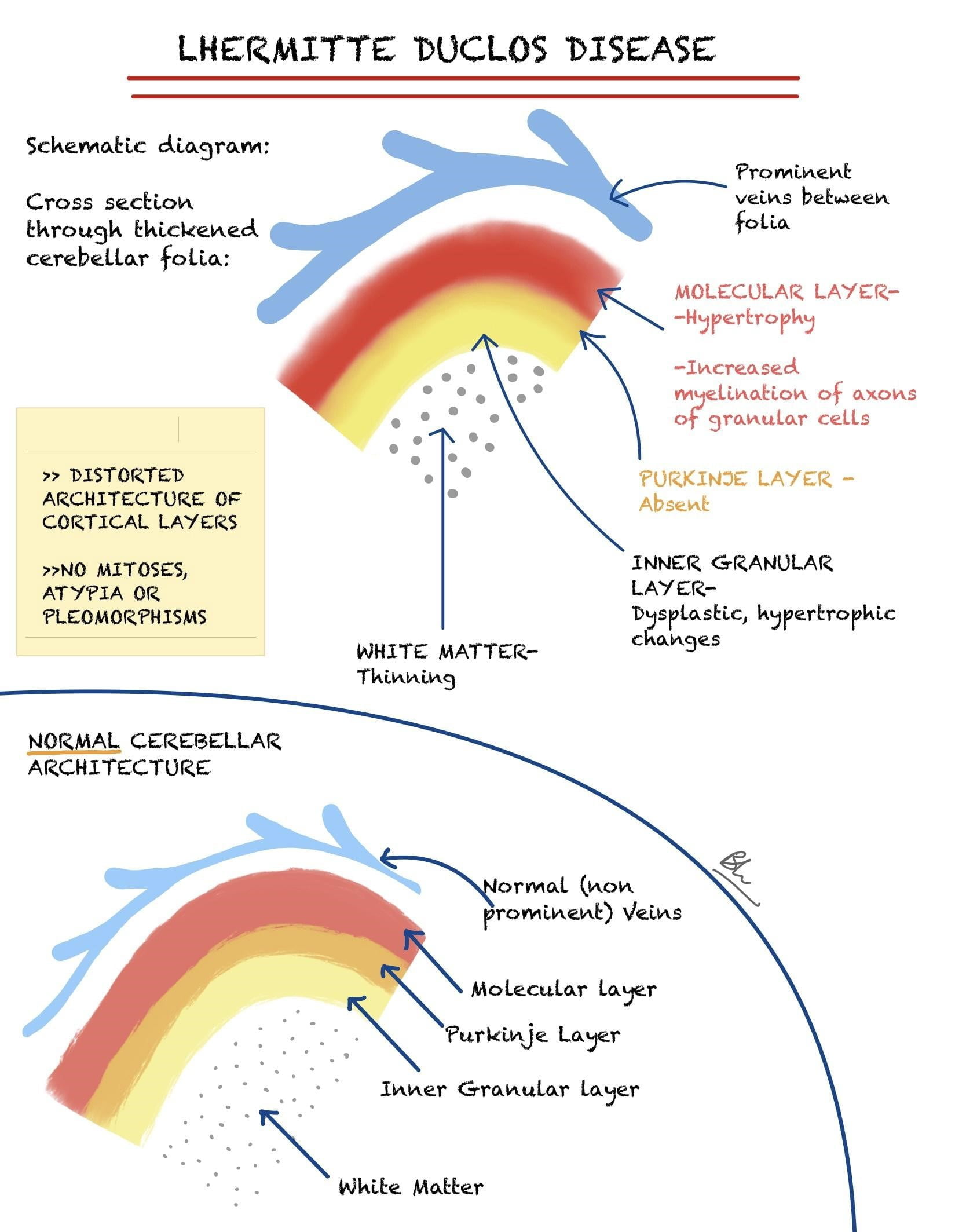
Location:
Always infratentorial. May involve the vermis or the cerebellar hemispheres. Unilateral cases are more common.
These lesions are often large and may displace the fourth ventricle and result in hydrocephalus.
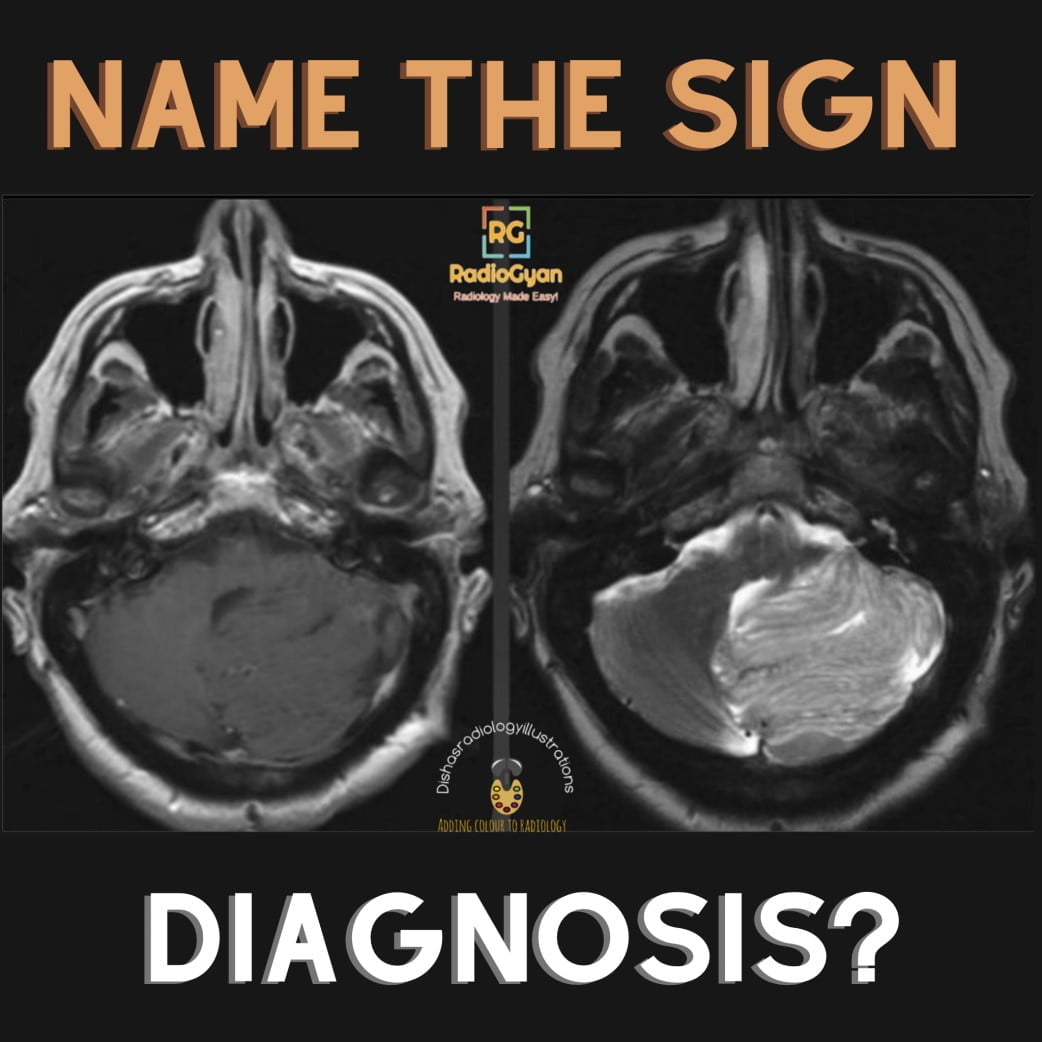
Key Imaging Features:
Cerebellar unilateral non enhancing lesion
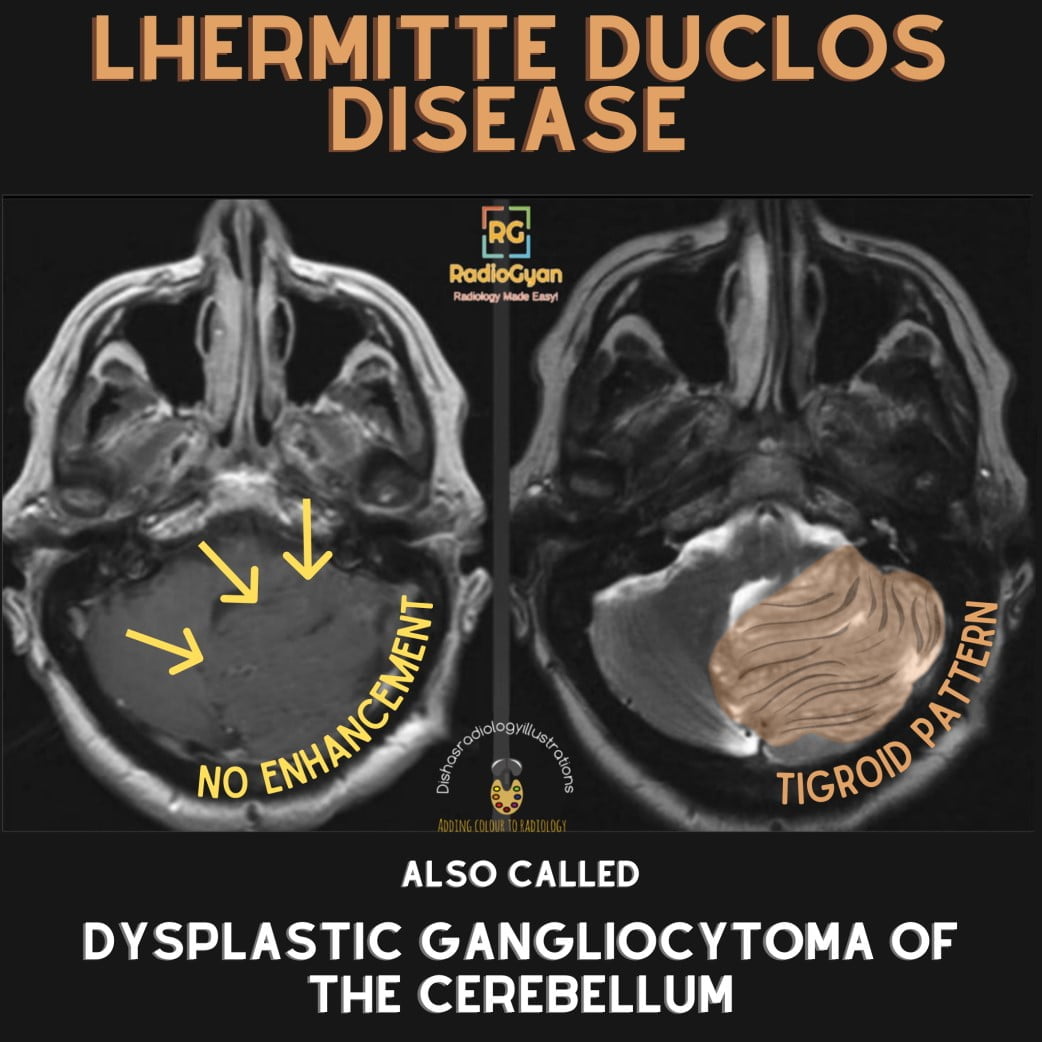
MRI:
Expansile mass, with-
- T1- Linear hypointense bands.
- T2- Alternating inner hyperintense and outer hypointense layers in enlarged cerebellar folia. Described as the pathognomic “Tiger Stripe” pattern/ corduroy pattern. Rarely, false positive tigroid patterns may be seen in Medulloblastoma, hence functional MR imaging is important.
- STIR– Lesion better delineated.
- T2* (GRE/SWI)- Prominent venous channels are seen around the enlarged folia.
- DWI– May show restricted diffusion, due to hypercellularity(T2 effect).
- ADC maps– Normal: helps in post operative differentiation in surgical margins and tumor (difficult to differentiate on T2 weighted images)
- Post-contrast- Linear enhancement of the abnormal veins between the folia.
- MR spectroscopy-
- Similar to usual characteristics of cerebral tumours: Reduced NAA(Normal or slightly reduced). A lactate doublet may be present (likely due to high glucose metabolism)
- Unlike usual cerebral tumour characteristics: Decreased or normal Cho/Cr and decreased myo-inositol/Cr ratios. No increase in lipids.
- Perfusion imaging- Increased relative cerebral volume, due to the enlarged veins (not due to malignancy, the lesion is nonmalignant)
- Fiber tractography- Helps map out tracts for surgery.
CT–
- Most of the lesions appear hypodense compared to a normal brain.
- Mass effect- Compression of fourth ventricle, effaced cerebellopontine cisterns and obstructive hydrocephalus are common.
- Calcification is not common. Necrotic or hemorrhagic changes are absent.
- The lesion does not show post-contrast enhancement.
Nuclear imaging:
FDG PET/ CT-
- The lesion is moderately hypermetabolic, in spite of not being a malignant lesion.
- This may be due to increased cellular density or different uptake.
SPECT –
Significant uptake of 201-Tl on SPECT.
Imaging Recommendation :
- For diagnosis: Contrast-enhanced MRI.
- For surgery planning: Fiber tractography.
- For follow up: Contrast-enhanced MRI. ADC maps are useful to differentiate recurrence from surgical changes.
- For screening of Cowden syndrome: Upper and lower gastrointestinal endoscopy.
Top Differential Diagnosis:
| Differential diagnosis | Features similar to LDD | Features distinct from LDD |
| 1.Medulloblastoma- Shh desmoplastic variant | Lateral cerebral mass, young population; very rare to find tiger stripe pattern | Tiger stripe pattern is mostly absent |
| 2.Cerebellar infarction | Cerebellar lesion, hyperintense on DWI images, Non enhancing | Acute or subacute onset (not gradual and chronic), confined to a vascular territory. |
| 3. Ganglioglioma | Posterior fossa lesion, rarely may show tigroid pattern | Enhancement seen |
| 4. Cerebellar cortical dysplasias | Posterior fossa lesion | Rarely cause hydrocephalus/ mass effect. Not gradually progressive. |
| 5. Tuberous sclerosis complex | Posterior fossa lesion | Younger age group, other evidence of tuberous sclerosis are present. |
Clinical Features :
- Symptoms– patients may be asymptomatic or may present with symptoms of increased intracranial pressure ( headache, nausea, vomiting). Other Symptoms may include cranial nerve palsies, gait abnormalities, and reduced visual acuity.
- Natural course: Lesions grow in size gradually over several years. No metastatic spread has been documented.
- Age/Sex predilection-. Most patients present in the age group 20 – 40 years.There is no gender predilection.
- Risk factors– 40% of the cases occur as a part of Cowden syndrome.
Classification System:
WHO grade I lesion.
Etymology and synonyms:
Other terms used to describe the condition are:
- Dysplastic cerebellar gangliocytoma,
- Granular cell hypertrophy,
- Granulomolecular hypertrophy of the cerebellum,
- Cerebellar hamartoma,
- Diffuse ganglioneuroma
- Gangliomatosis of the cerebellum.
Management:
Treatment:
- Debulking procedures/ shunting to relieve obstruction: in patients with symptoms or obstructive hydrocephalus.
- Common complications-
- Complete resection is challenging as the tumor does not have a defined capsule.
- ‘Cerebellar mutism’ post-surgery.
- Recurrence of lesion post-surgery even after prolonged disease-free periods
Screening:
- To rule out concomitant malignancies (Upper and lower gastrointestinal endoscopy), as Cowden Syndrome is a common coexistence.
References:
Single best review article:
- Klisch, J. (2001) ‘Lhermitte-Duclos Disease: Assessment with MR Imaging, Positron Emission Tomography, Single-photon Emission CT, and MR Spectroscopy’, American Journal of Neuroradiology, 5, pp. 824–830.
Other references:
- ● Osborn, Anne (2017) ‘Neoplasms, cysts and tumor like lesions’, in Osborn’s brain imaging, pathology and anatomy. 2nd edn. Elsevier, pp. 598–601.
- Hilario, A. (2018b) Lhermitte-Duclos disease: typical MRI findings, Neuroradiology. doi:10.1594/EURORAD/CASE.15399.
- Borni, M. et al. (2019) ‘The Lhermitte-Duclos Disease: A rare bilateral cerebellar location of a rare pathology’, Pan African Medical Journal, 33. doi:10.11604/pamj.2019.33.118.16809.
Case co-authored by TeamGyan Member Dr Bhargavi Sovani.
Illustration by Dr. Disha Lokhandwala.