Quiz
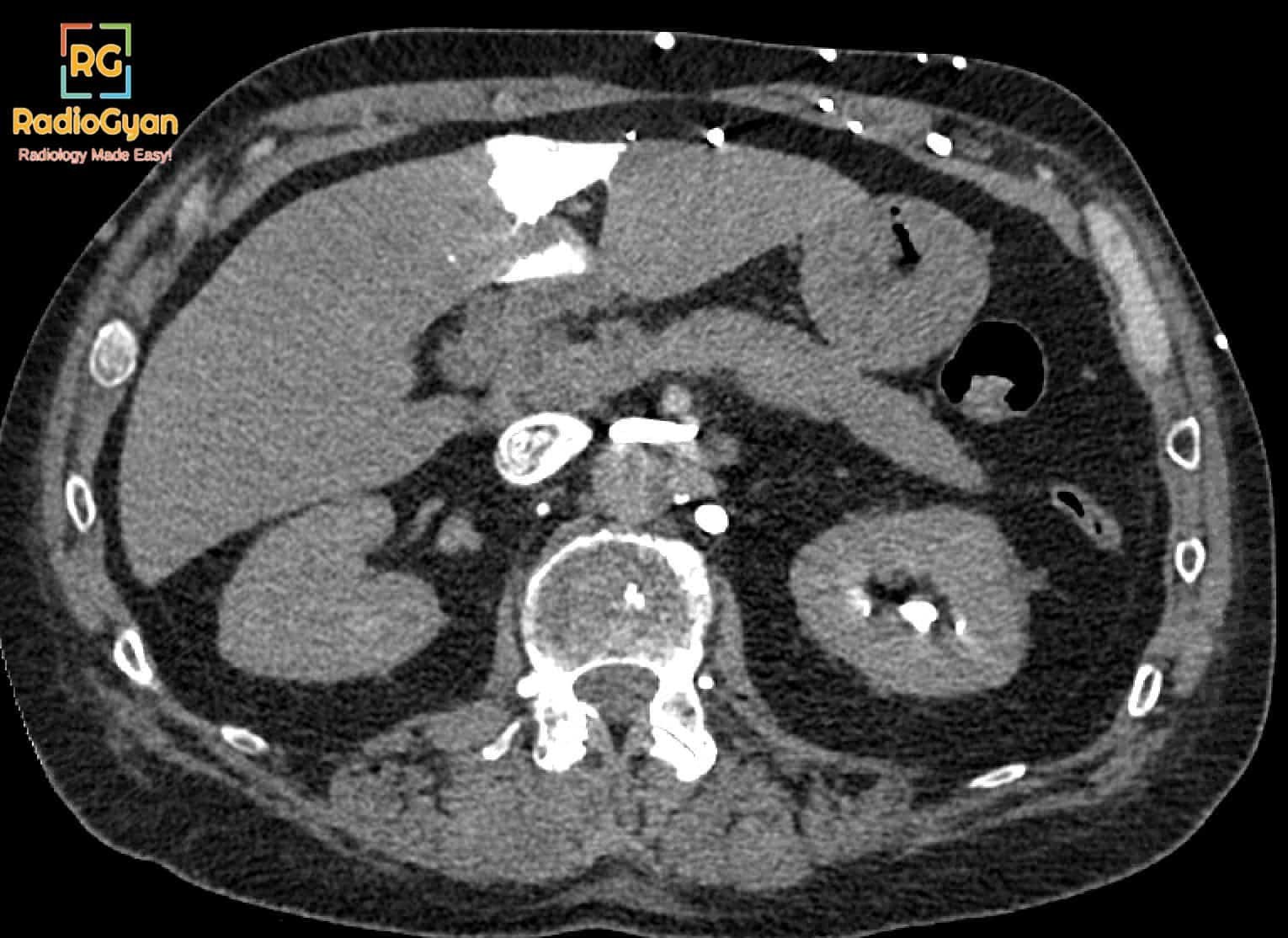
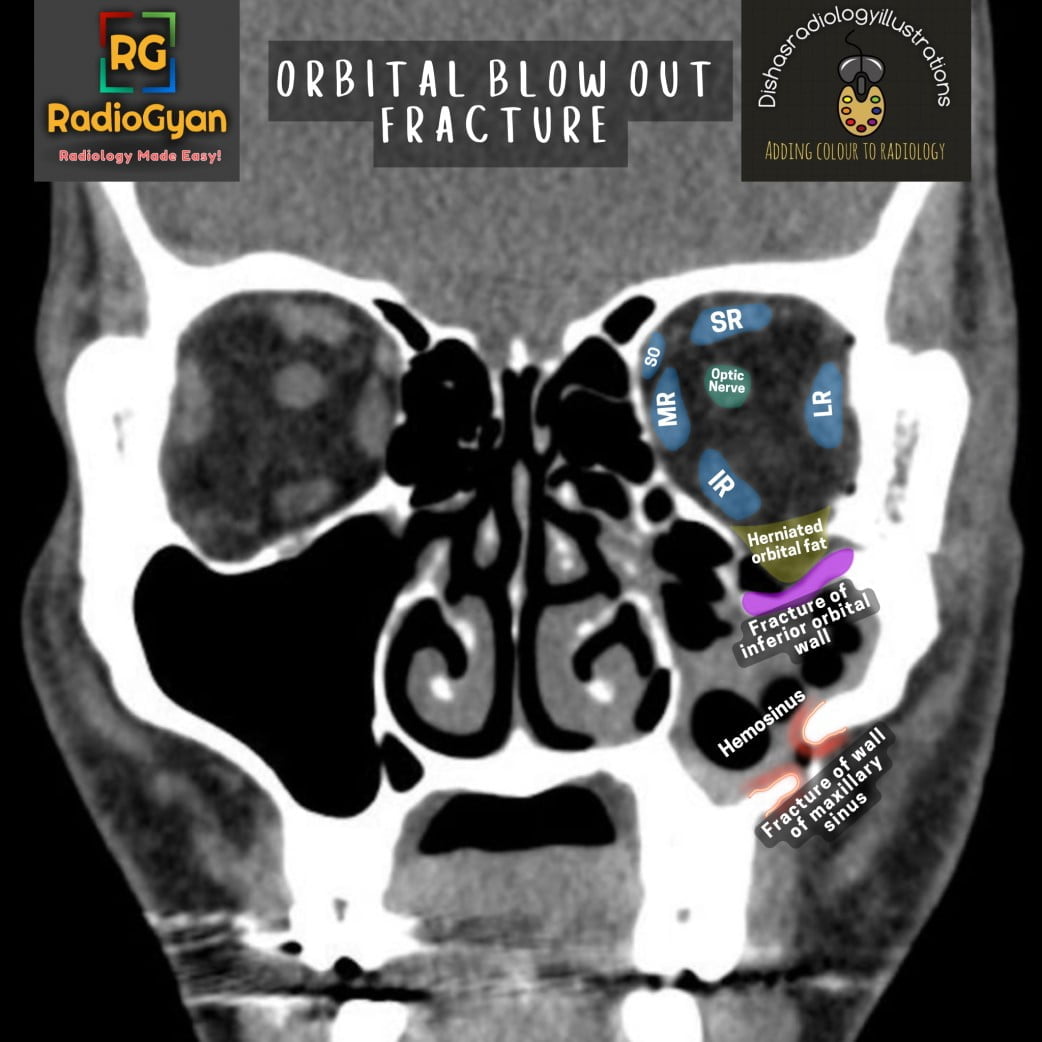
Which of the following is NOT a feature of this pathology?
- Fracture of medial orbital wall.
- Entrapment of extraocular muscles.
- Herniation of orbital fat.
- Fracture of inferior orbital rim.
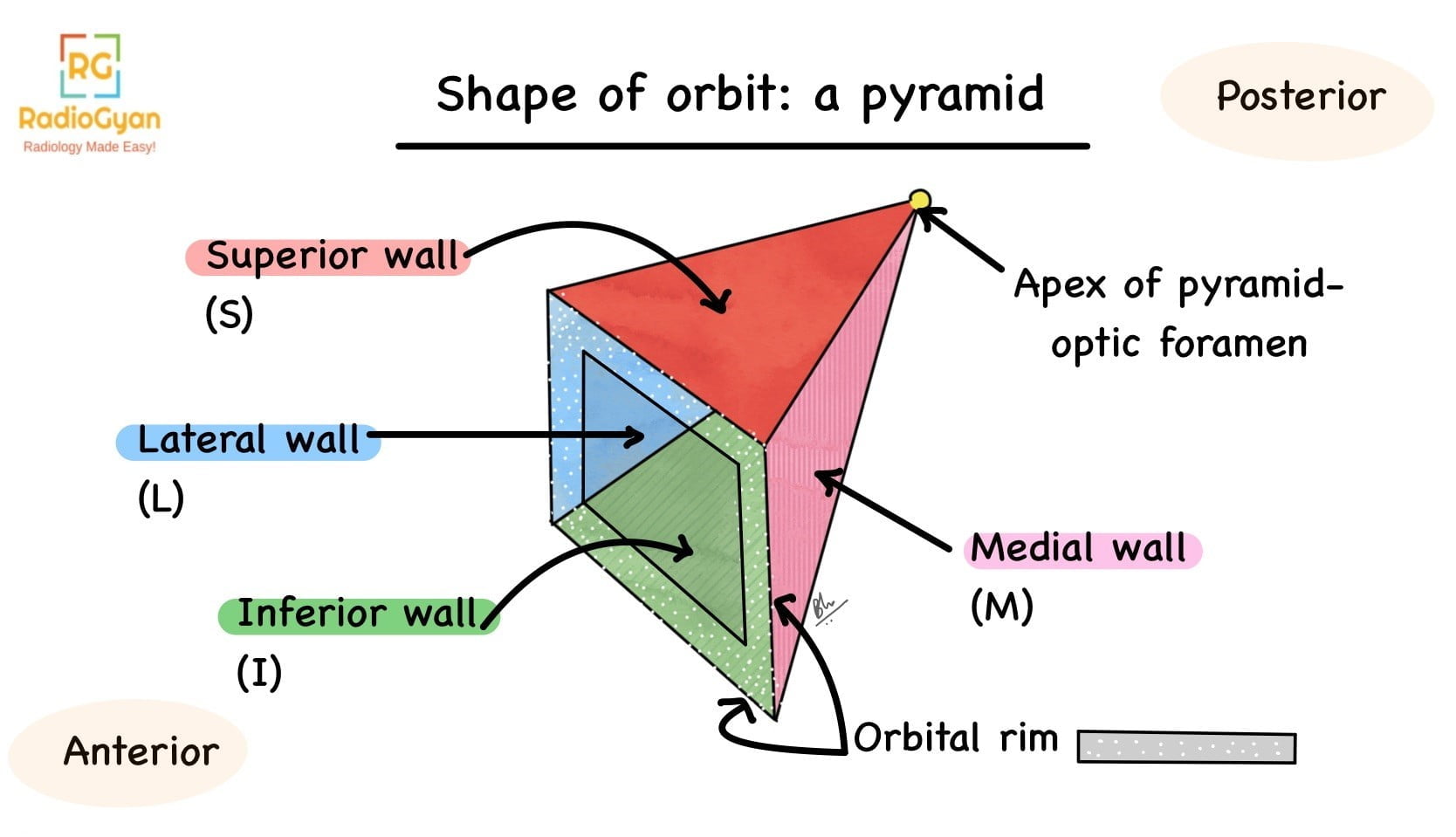
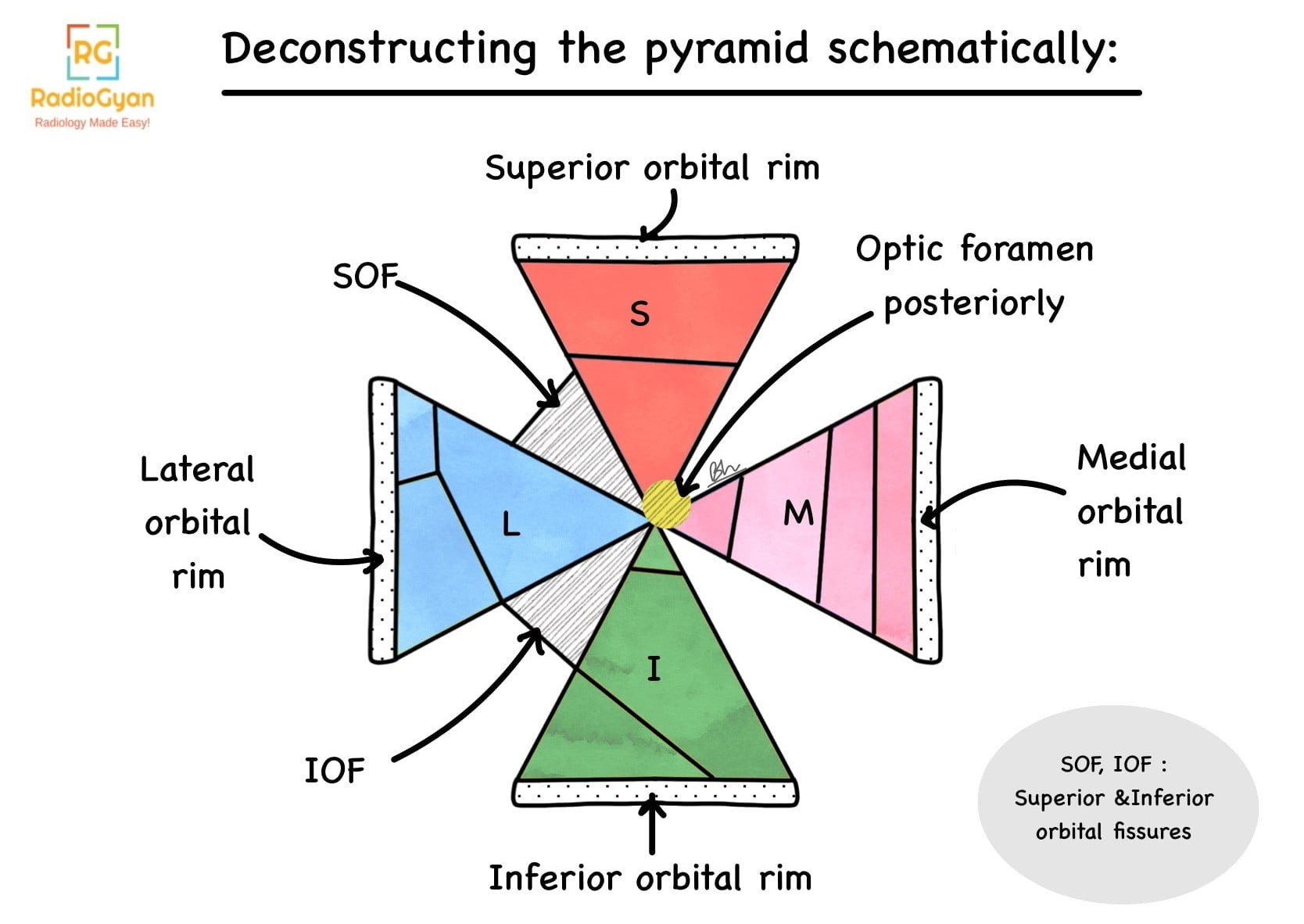
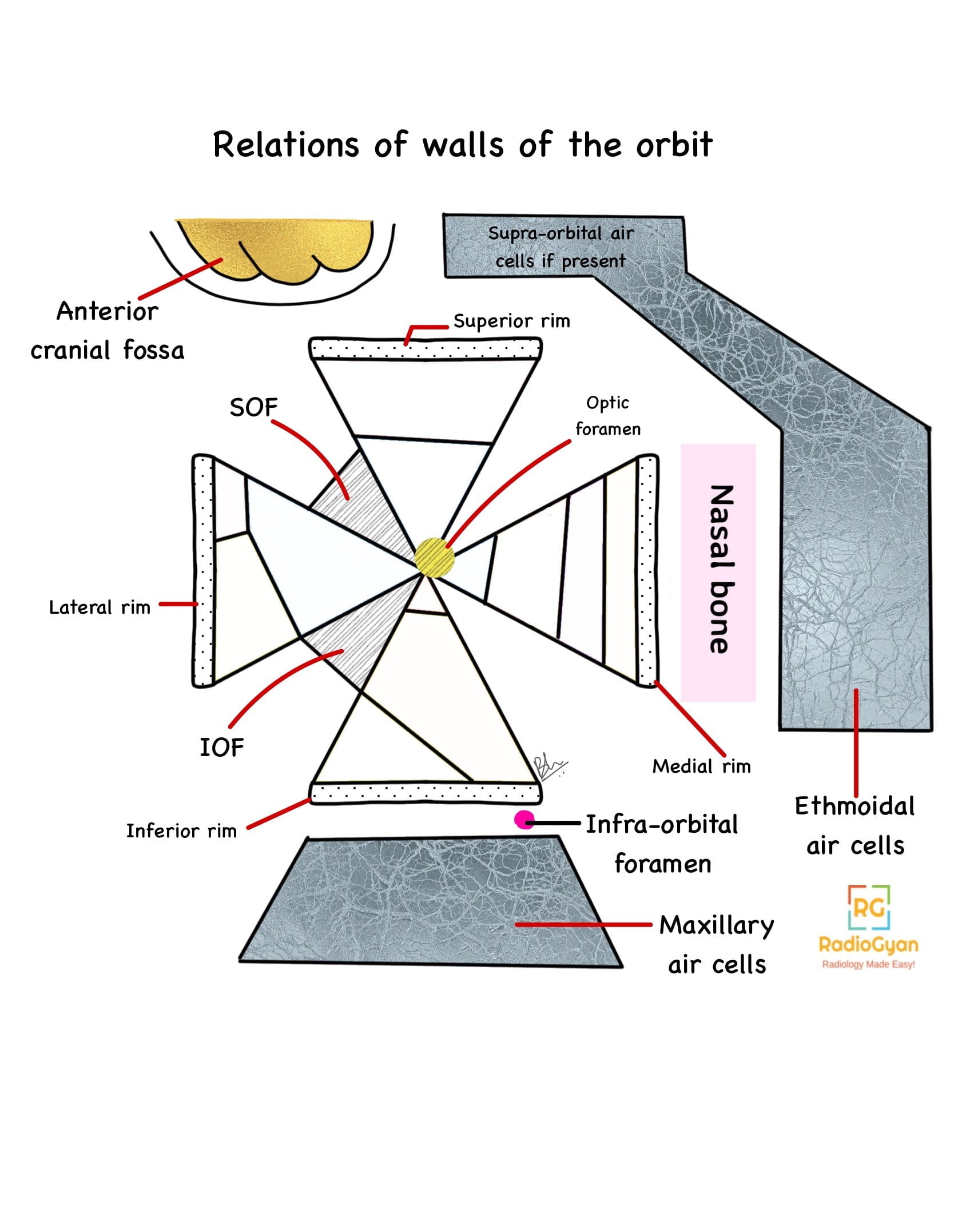
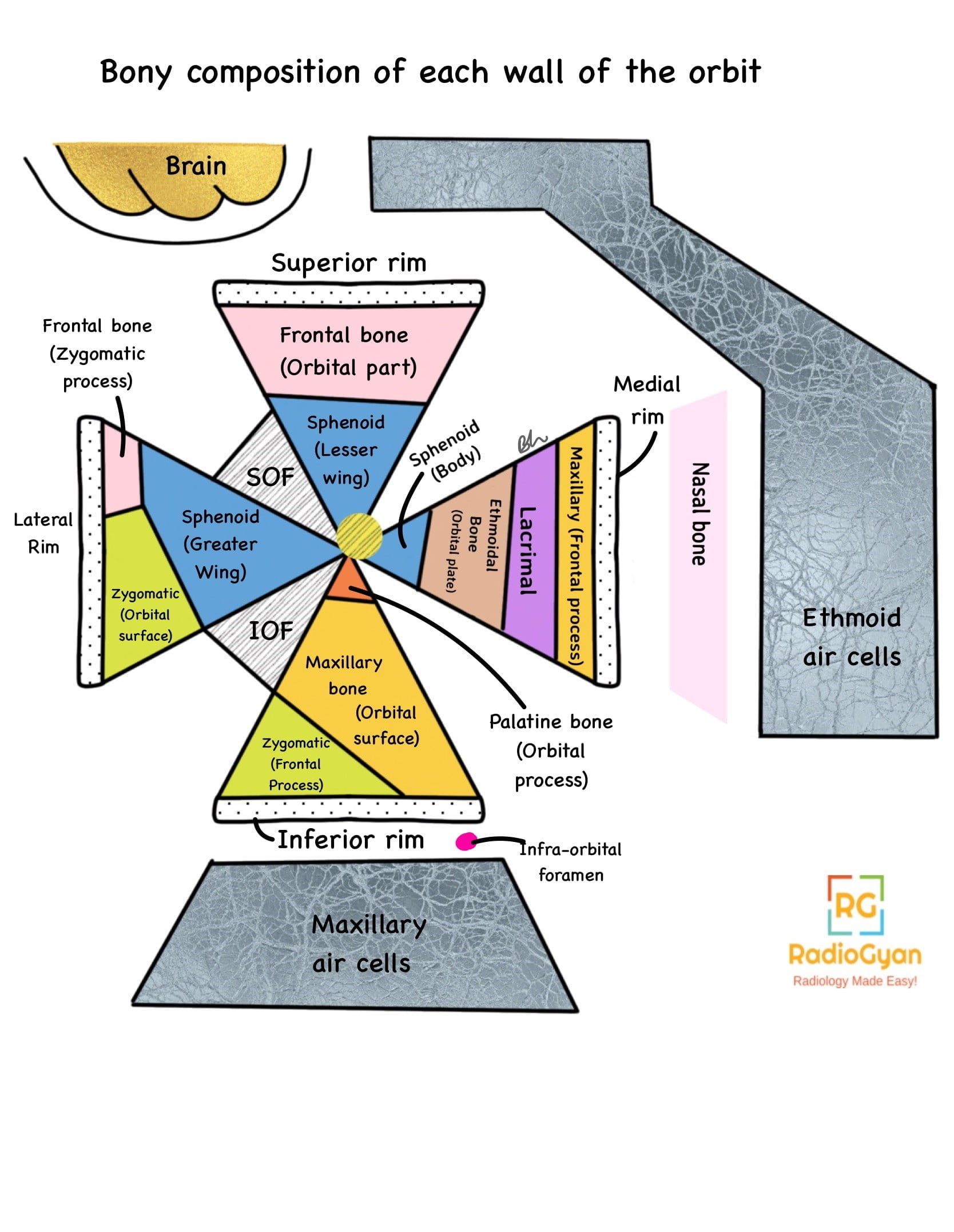
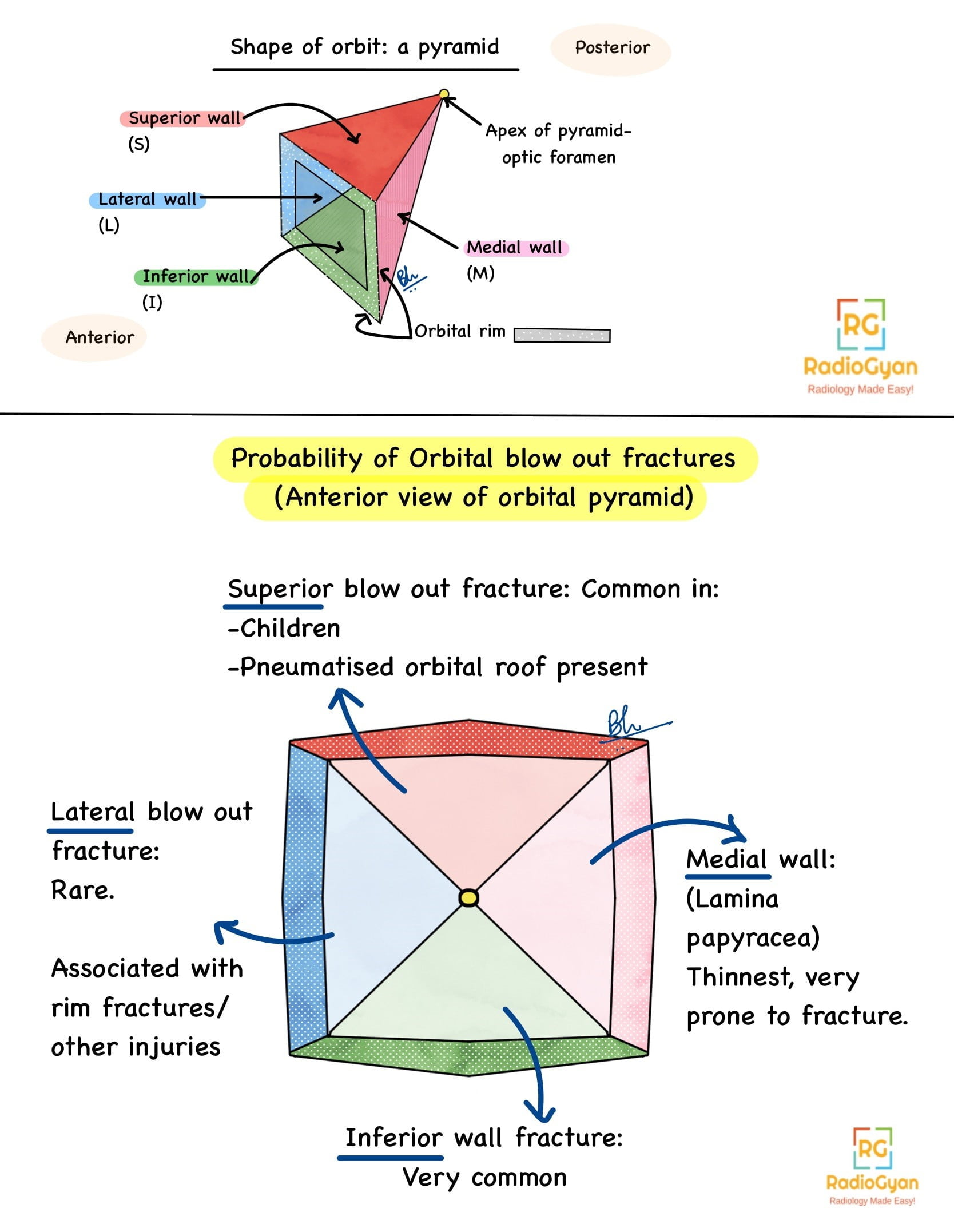
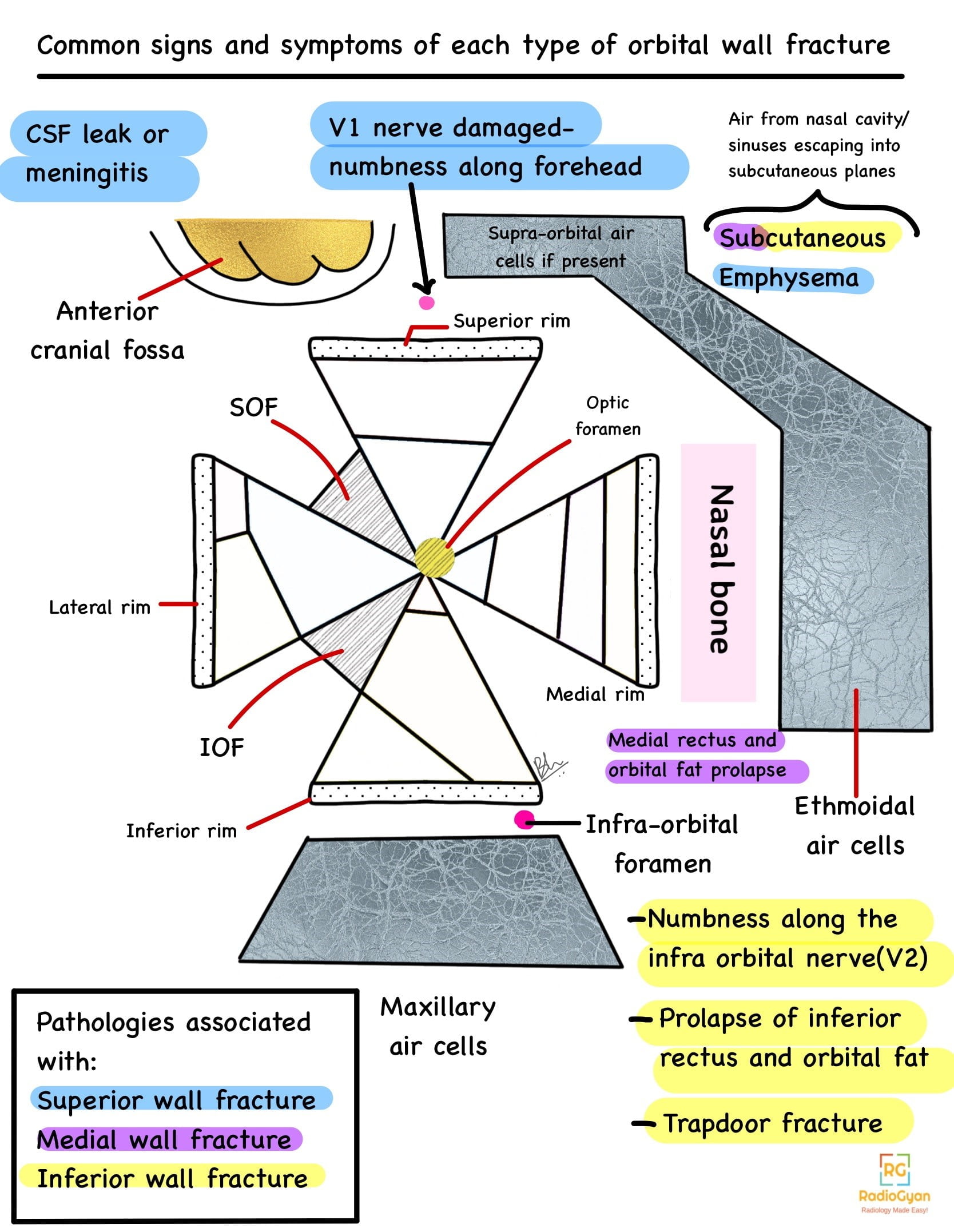
To understand the pathologies associated with orbital blow out fractures, let us first review the anatomy of the orbit in brief.
Anatomy of the orbit:
Colle fracture is characterized as an extra-articular fracture of the radial metaphysis caused by a fall on an outstretched hand (FOOSH), typically pronated forearm in wrist extension) causing dorsal angulation of the distal fracture fragment.
Key Imaging Features
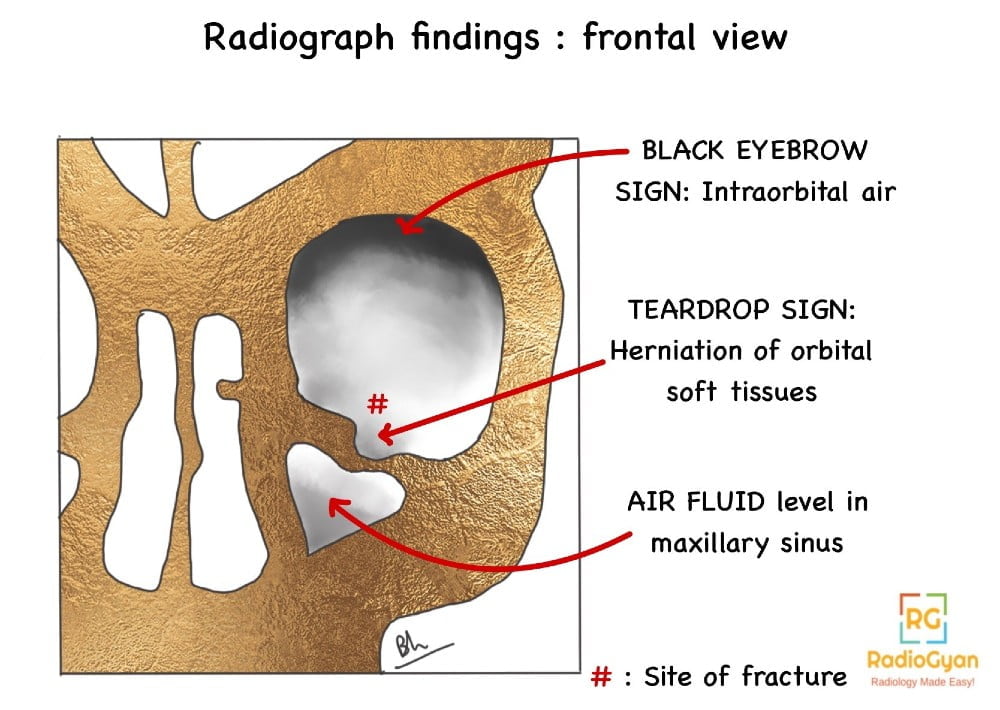
- Radiograph: Frontal PA or AP view, Caldwell, Waters, Towne and lateral views.
- Black eyebrow sign: Air in the superior aspect of the orbit, appears like an eyebrow.
- Soft tissue teardrop sign: along the roof of maxillary sinus.
- Air fluid level in the maxillary sinus.
CT : Study of choice.
- Thin images (less than or equal to 3mm), bone window and non contrast images.
- Axial, Sagittal images: To gauge distance between fracture and apex of the orbit. If medial wall fracture extends uptill within 1 cm of the optic canal, the optic nerve is at more risk of entrapment during surgery, and must be approached with more caution.
- Coronal images: To gauge extent, direction of fracture, especially for floor and roof fractures. Also helps assess change in shape of orbit.
- Thicker slices with soft tissue windowing to assess soft tissue injury like retrobulbar fluid, subperiosteal bleeding, extraocular muscles, optic nerve injury. Maxillary hemosinus predicts orbital floor fracture (negative predictive value 99.7% according to Huang et al.)
- Multiplanar reconstruction, 3D reconstructions to assess asymmetry, and to provide surgical guidance.
- Orbital volume measurement to assess for increased volume secondary to widening caused by fracture. Once the edema settles down, there is an increased probability of enophthalmos.
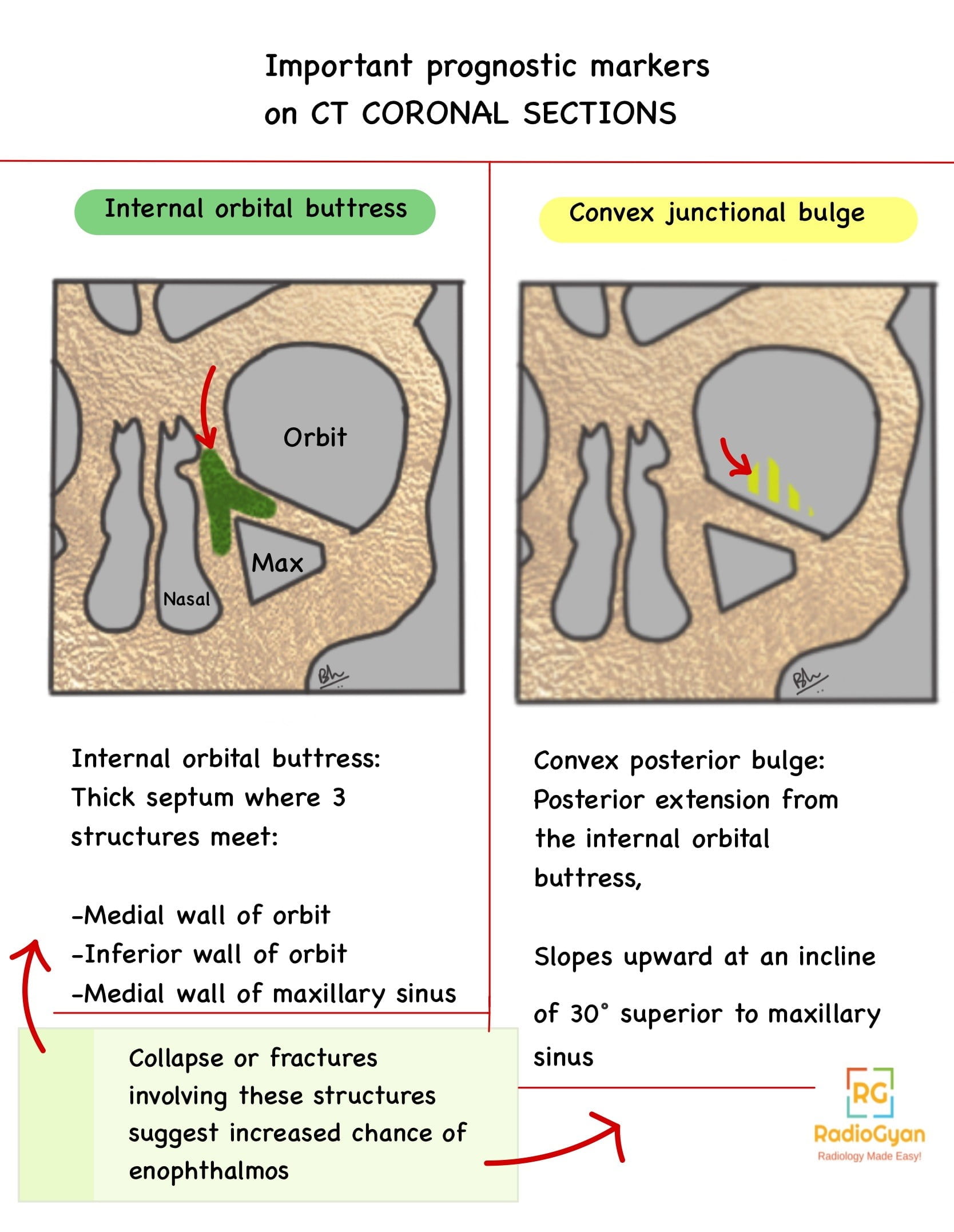
- Increased chance of late enophthalmos is predicted based on following CT findings:
- Fracture area ≥2 cm²
- Involvement of medial or inferior wall in fracture ≥25 to 50 %
- Collapsed internal orbital buttress or convex junctional bulge
- Soft tissue herniated through defect, volume > 1.5 ml (each 1 ml of volume displacement corresponds to 0.9 ml of enophthalmos.)
A guide to where to look for the ‘internal orbital buttress’ or ‘convex junctional bulge’ is shown in the image that follows:
- CT also helps rule out foreign bodies and establish the material of the foreign bodies if present. For eg. a foreign body of wood: -100 to -200 HU, overtime increases in density when fluid (edema) accumulates.
- MRI :
- T2 weighted images, Contrast enhanced fat suppressed MR images.
- Must exclude iron containing foreign bodies before MRI.
- Injuries of the globe, subperiosteal bleeding, retrobulbar fluid, optic nerve
- Ultrasound: May be used to visualise intraocular structures
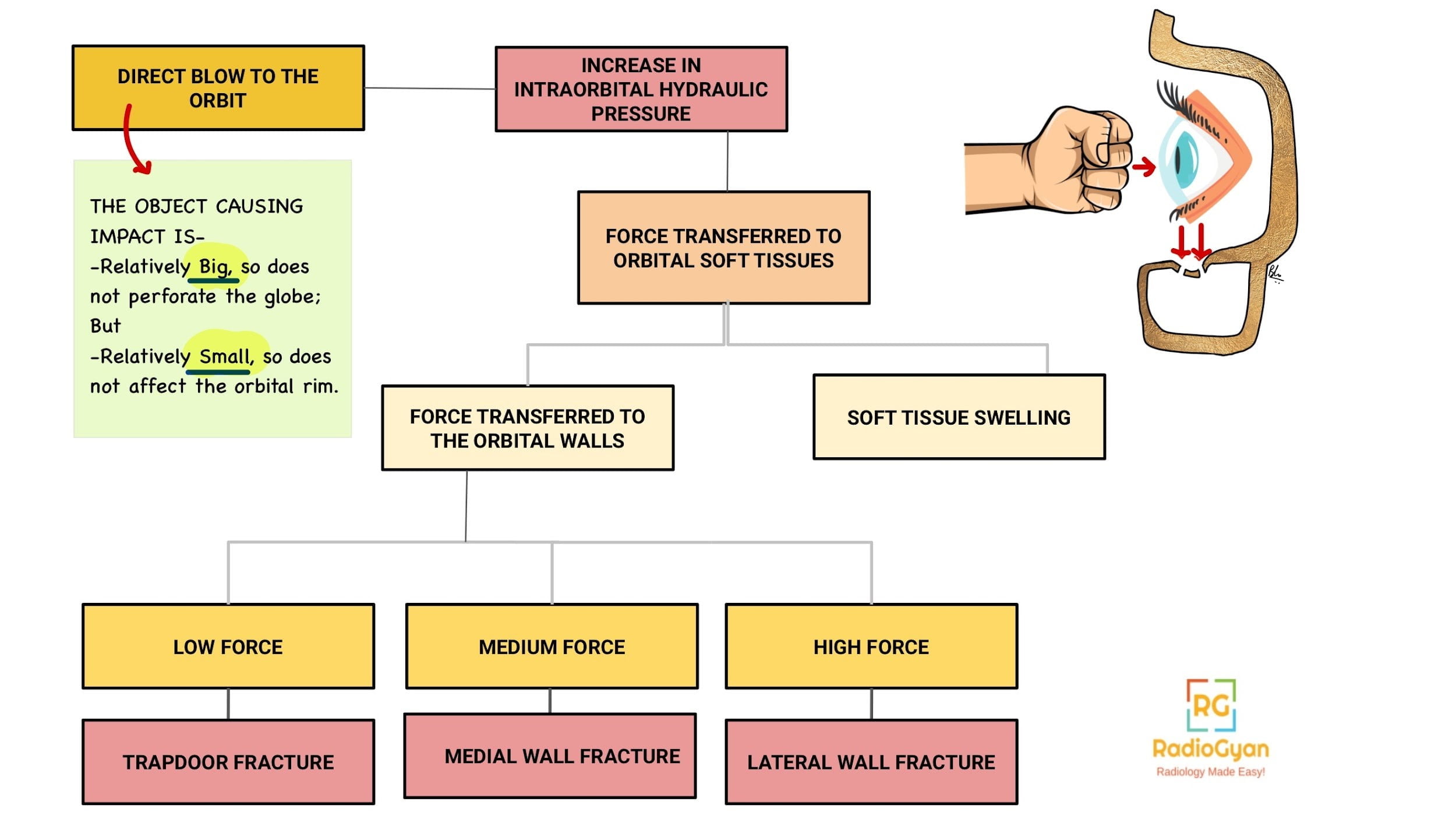
Pathophysiology:
Fracture of the walls of the orbit with an intact orbital rim, is called a blow out fracture.
Mechanism of injury:
Imaging Recommendation :
HRCT scans with thin sections, coronal views, bone and soft tissue windowing, multiplanar reconstructions.
Top 3 Differential Diagnosis:
- Orbital haematoma.
- Other orbital fractures.
- Congenital dehiscence of lamina papyracea.
Clinical Features:
- Symptoms:
- Decreased visual acuity.
- Enophthalmos- Posterior displacement of intact eye globe.
- Diplopia- Due to extraocular muscle entrapment.
- Orbital emphysema – If fracture into the paranasal sinuses.
- Paresthesias along the malar region – Due to infra orbital nerve injury.
- Epistaxis, eye swelling, especially on exerting force ( like nose blowing.)
- Deepened supraorbital crease, narrowing palpebral fissure.
- Age/Sex predilection: More common in young males, as they are more prone to orbital trauma. May also be a result of intimate patient violence in females.
- Association with: Zygomatic arch fractures, Le Fort type II or III, other orbital fractures.
Classification System:
A)Broadly classified as:
- Open door fractures: Large, displaced, comminuted. May have minimal diplopia (Absence of muscle entrapment due to absence of small defects like in the case of trapdoor fractures).
- Thus absence of diplopia should not give a false sense of assurance of lesser severity of injury.
- Trapdoor fractures: Linear, hinged, minimally displaced.The sequence of pathologies are described as follows:

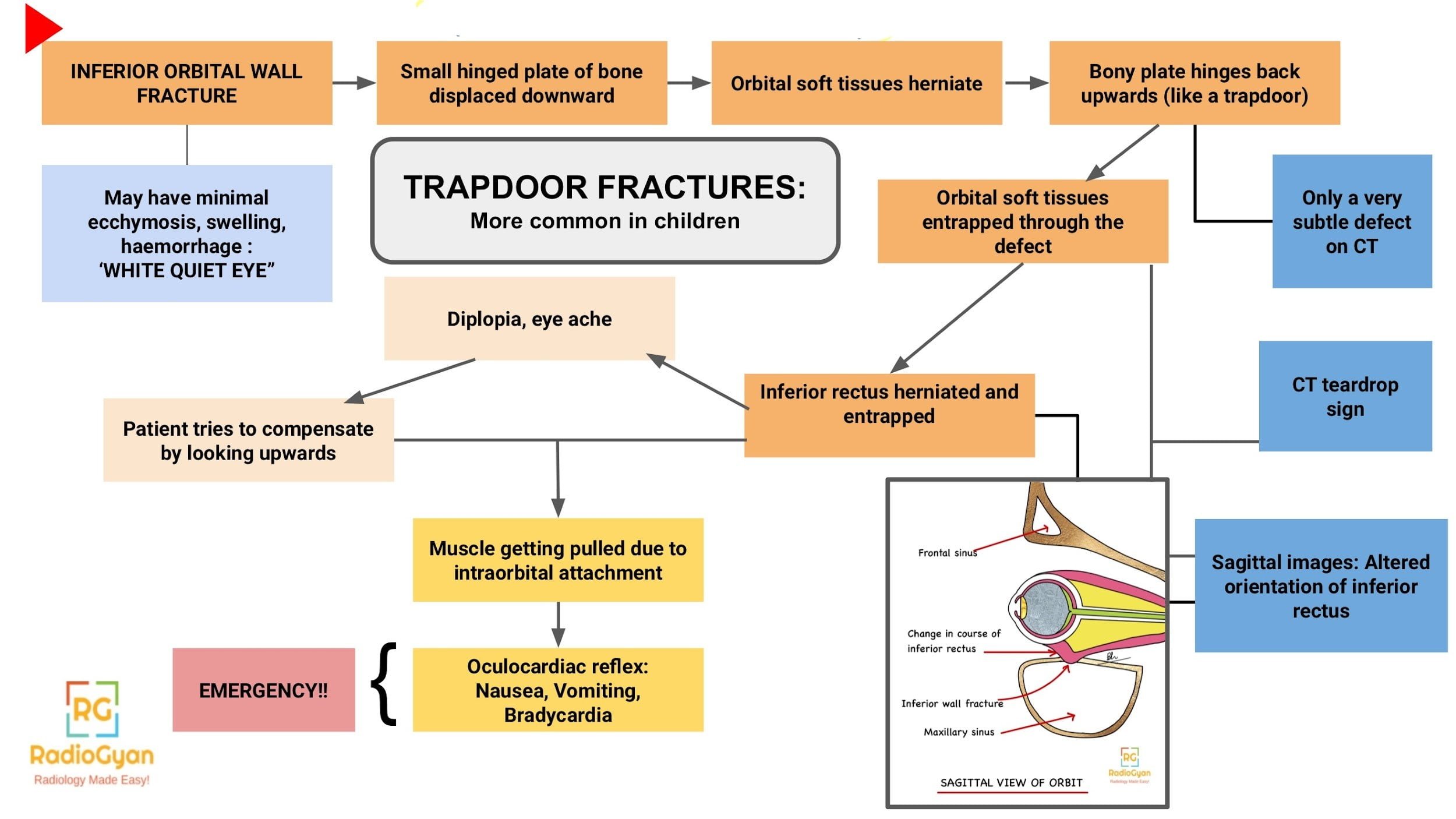
B) Isolated orbital floor OR medial wall fractures are classified as:
- Hinged: A bent part of the blown out fragment is attached due to intact periosteum; a possibility in floor fractures.
- Punched Out: Entire fractured fragment is free, more common in medial wall fractures.
C) Combined orbital floor + medial wall fractures are classified as:
- Simple: No collapse of internal orbital buttress. ( around 60 %)
- Complex: Collapse of internal orbital buttress and junctional bulge, suggesting more significant changes in orbital volume, and loss of bony landmarks during surgical reconstruction. This is important to establish on preoperative CT to guide the use of specific implants suited for this condition.
A guide to where to look for the ‘internal orbital buttress’ or ‘convex junctional bulge’ is shown in the image under CT findings.
Etymology and synonyms :
Called blow out fracture due to the nature of injury of fractures to the walls of orbit.
Treatment :
- Immediate physical examination and high resolution CT is warranted.
- Urgent lateral canthotomy and oral prednisone treatment if signs of increased intraocular pressure.
- Medical therapy: Absence of the following features qualify for medical therapy-
- Significant enophthalmos (less than 2mm)
- Fracture of > 50 % orbital floor
- Marked hypo-ophthalmos
- Entrapped muscle or orbital tissue.
- Diplopia
- Medical therapy includes oral antibiotics, short course of oral steroids as needed.
- Surgical therapy: Above mentioned severe features warrant surgical intervention. Surgery within 2 weeks of injury prevents fibrosis. Post operative CT is important to identify entrapment to prompt revision surgery.
- Interspecialty approaches with a joint team of an ophthalmologist, otolaryngologist, plastic surgeon, maxillofacial surgeon is suggested.
- Observation and follow up even after discharge is important.
References:
Single best review article:
Other references:
- Koenen L, Waseem M. Orbital Floor Fracture. [Updated 2022 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
- Nguyen, V.D. et al. (2017) ‘Demystifying orbital emergencies: A pictorial review’, RadioGraphics, 37(3), pp. 947–962. doi:10.1148/rg.2017160119.
- Adam J Cohen, M. (2023) Orbital floor fractures (blowout), Practice Essentials, History of the Procedure, Problem.
- Blowout! managing the orbital floor fracture (2016) American Academy of Ophthalmology.
- Al-Qattan, Mohammad M. , MBBS*; Al-Qattan, Yousef M.†. “Trap Door” Orbital Floor Fractures in Adults: Are They Different from Pediatric Fractures?. Plastic and Reconstructive Surgery – Global Open 9(4):p e3537, April 2021. | DOI: 10.1097/GOX.0000000000003537
- Kubal WS. Imaging of orbital trauma. Radiographics. 2008 Oct;28(6):1729-39. doi: 10.1148/rg.286085523. PMID: 18936032.
- Iowa head and Neck Protocols Facial Fracture Management Handbook – Orbital blowout fractures | Iowa Head and Neck Protocols.
Case co-authored by TeamGyan Member Dr.Bhargavi Sovani.
Illustrations by Dr Bhargavi Sovani.
Annotated image by Dr Disha Lokhandwala.