Disclaimer: The author makes no claims of the accuracy of the information contained herein; this information is for educational purposes only and is not a substitute for clinical judgment. This calculator is based upon the American College of Radiology (ACR) classification, but this calculator is not officially endorsed by the ACR. Kindly refer to the ACR website for latest updates.
Menupausal Status?
You can hover over/click a few tabs for illustrations for eg. Time intensity curves.
More useful tools:
Introduction to O-RADS MRI
The Ovarian-Adnexal Reporting Data System Magnetic Resonance Imaging (O-RADS MRI) is a critical tool in the evaluation of indeterminate ovarian masses. This scoring system is designed to help healthcare professionals categorize these masses based on their risk of malignancy, facilitating appropriate management strategies. Given that a significant percentage of ovarian masses are indeterminate on transvaginal ultrasound, the O-RADS MRI score plays an essential role in guiding clinical decisions and improving patient outcomes.
Importance of O-RADS MRI
Clinical Relevance
Finding an incidental ovarian mass is a common occurrence in women, especially during imaging for unrelated conditions. Studies indicate that up to 30% of these masses may be classified as indeterminate after initial imaging. Traditional methods, such as percutaneous biopsy, carry risks, including potential tumor dissemination and poor diagnostic performance. As a result, many patients may undergo unnecessary surgeries, leading to increased morbidity and potential loss of fertility.
The application of the O-RADS MRI score provides a structured approach to categorizing these masses, allowing healthcare providers to reduce unnecessary interventions. By accurately stratifying the risk of malignancy, clinicians can ensure that women with benign masses receive appropriate care while promptly referring those with malignant or borderline tumors to specialized oncology centers.
Patient Outcomes
The effective use of the O-RADS MRI score contributes to improved patient outcomes by:
- Reducing Unnecessary Surgeries: By accurately identifying benign masses, patients can avoid the risks associated with invasive surgical procedures.
- Enhancing Referral Processes: Patients with suspected malignant masses can be quickly referred to specialized care, ensuring timely intervention and better survival rates.
- Improving Patient Education: The O-RADS MRI system provides clear criteria that can help educate patients about their conditions, fostering informed decision-making regarding their treatment options.
Categories of the O-RADS MRI Score
The O-RADS MRI score divides ovarian masses into five distinct categories based on the risk of preoperative malignancy:
- Score 1: This category includes normal ovarian cysts (such as follicles) and extra-ovarian masses. These findings are typically benign and do not require further intervention.
- Scores 2-3: These scores correspond to benign ovarian masses that are very unlikely to be malignant. They have a negative predictive value for malignancy of approximately 98%. Lesions in this category can be safely managed in non-cancer centers using minimally invasive surgical techniques.
- Scores 4-5: These categories correspond to borderline or malignant tumors. Scores 4 and 5 indicate a higher risk of malignancy and should prompt referral to tertiary care centers for specialized oncological surgery. The sensitivity and specificity of these scores are high, making them reliable indicators for further action.
Visual Representation of Categories
| O-RADS Score | Description | Management Recommendations |
|---|---|---|
| Score 1 | Normal cysts or extra-ovarian masses | No action required |
| Scores 2-3 | Benign ovarian masses | Managed in non-cancer centers |
| Scores 4-5 | Borderline or malignant tumors | Refer to specialized oncology centers |
MRI Protocol for O-RADS Scoring
Applying the O-RADS MRI score requires adherence to a standardized MRI protocol to ensure accurate characterization of ovarian masses. The following imaging sequences are recommended:
- T2-weighted images: Acquired in both axial and sagittal/coronal planes with a slice thickness of 4 mm. This sequence provides critical information regarding the morphology and internal characteristics of the mass.
- T1-weighted images: Axial views should be performed with a slice thickness of 3 mm. T1-weighted images assist in assessing fat content and other tissue characteristics.
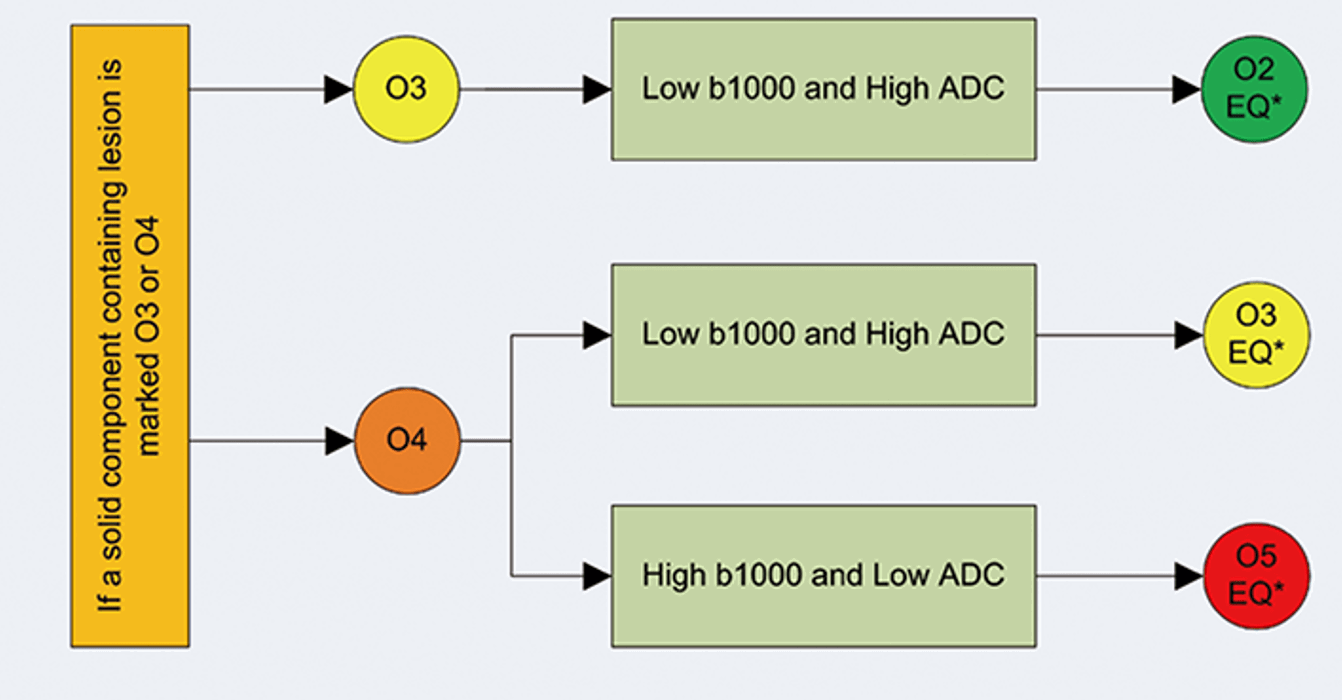
- Diffusion-weighted imaging (DWI): Utilizing b1000 and ADC maps with a slice thickness of 4 mm, DWI is crucial for evaluating the cellularity of the mass.
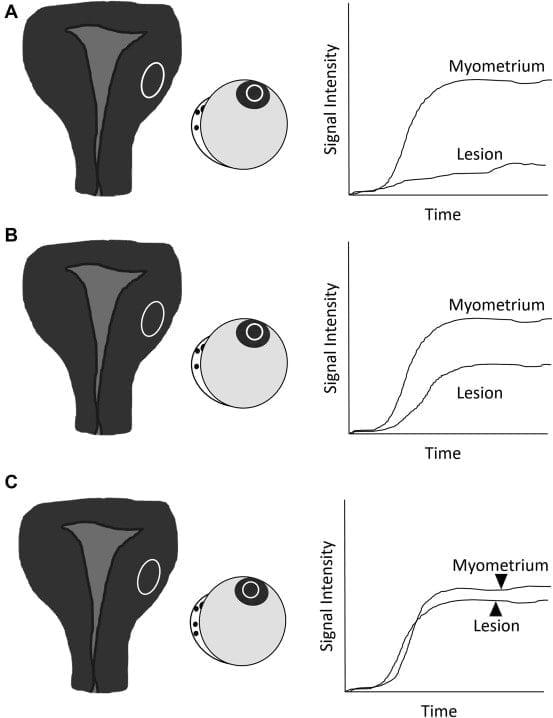
- Dynamic contrast-enhanced sequences: This sequence is key for assessing time-intensity curves (TIC), which reflect how the mass absorbs contrast over time. Dynamic imaging should ideally start 30 seconds before contrast injection and continue for four minutes afterward.
These imaging sequences are essential for differentiating benign from malignant masses based on their characteristics and behavior during imaging.
Common Errors in O-RADS MRI Application
Despite its effectiveness, healthcare professionals must be aware of common pitfalls when using the O-RADS MRI scoring system:
- Misinterpretation of Normal Variants: Healthy ovarian tissue may exhibit characteristics that resemble solid masses. Understanding the typical appearance of normal ovarian structures is crucial to avoid misclassification.
- Overlapping Imaging Features: Pelvic masses may have overlapping features with ovarian masses, leading to diagnostic confusion. Radiologists should carefully evaluate all available imaging data before concluding.
- Inaccurate Assessment of Dynamic Contrast Uptake Curves: The assessment of TIC can be subjective; therefore, radiologists must familiarize themselves with common patterns to avoid misclassification.
Strategies for Minimizing Errors
To mitigate these errors, radiologists can undertake the following steps:
- Continuous Education: Regular training sessions focused on O-RADS MRI scoring can enhance understanding and accuracy among radiologists.
- Utilization of Checklists: Using checklists during evaluations can help ensure that all necessary criteria are assessed before finalizing a diagnosis.
- Peer Review and Consultation: Engaging in peer reviews and seeking consultations from colleagues can provide additional perspectives and reduce misinterpretations.
Conclusion
The O-RADS MRI scoring system is an invaluable resource in managing indeterminate ovarian masses. By providing a structured approach to risk stratification and standardized imaging protocols, it enhances clinical decision-making and optimizes patient care. Practitioners looking to implement this scoring system must undergo thorough training and familiarize themselves with the associated imaging characteristics for effective application in everyday practice.
Future Directions
As advancements in imaging technology continue, future iterations of the O-RADS MRI system may incorporate additional parameters or refined categories based on ongoing research. Continuous evaluation and updating of the criteria will be essential to maintain its relevance and effectiveness in clinical practice.
For more information on using the O-RADS MRI calculator and to explore further resources, visit our dedicated webpage.
References
- O-RADS MRI Risk Stratification System: Guide for Assessing Adnexal Lesions from the ACR O-RADS Committee Elizabeth A. Sadowski, Isabelle Thomassin-Naggara, Andrea Rockall, Katherine E. Maturen, Rosemarie Forstner, Priyanka Jha, Stephanie Nougaret, Evan S. Siegelman, and Caroline ReinholdRadiology 2022 303:1, 35-47
- Mohamadian A, Moradi B. Simplified Approach for Ovarian-Adnexal Reporting and Data System MRI Risk Stratification System. Korean J Radiol. 2022 Nov;23(11):1115-1117. https://doi.org/10.3348/kjr.2022.0489CopyDownload Download with Abstract