Interventional Radiology (IR), also referred to as ‘Interventionology,’ is progressively advancing towards achieving independent specialty status, albeit its recognition varies globally. In certain regions, it continues to exist within a somewhat ambiguous framework or within diagnostic radiology. The absence of dedicated IR suites in many hospitals poses a significant challenge for residents seeking to gain comprehensive insights into this cutting-edge and technologically advanced field of medicine.
Approximately five years ago, we conducted a survey within our social media groups to assess the status of IR awareness. The findings underscored a noteworthy statistic; only 50% of the respondents indicated the presence of a dedicated IR department within their respective institutions.


Only a quarter of the residents had some knowledge about IR while the rest had zero knowledge.
The figures are worse for medical residents as they have little to no exposure to IR. In a recent study, Agarwal et.al. found that 60% of students cited a very poor/poor knowledge of IR, which is in line with multiple other studies.
So we requested Dr. Bibin Sebastian, an Interventional Radiologist to answer a few commonly asked questions about Interventional Radiology to help out radiology residents in 2019 and is now updated with a lot of new advancements in the field in 2024.
Interventional Radiology – Basics
What is interventional radiology and who is an interventional radiologist?

Interventional Radiology is a clinical branch of medicine which deals with a variety of therapeutic and diagnostic procedures that are performed using minimally invasive image-guided techniques.
Interventional radiologists are highly specialised physicians with expertise in imaging diagnosis and targeted minimally invasive treatments. Mastery in this field demands a profound understanding of imaging techniques and physics with a focus on radiation safety and hazards, knowledge of the pathologic basis of various disease conditions and its clinical presentation, and a comprehensive knowledge of radiation equipment—most of which aligns with the machinery employed in diagnostic radiology.
IRs are inherently radiologists who have successfully completed their core radiology training. Beyond their diagnostic proficiency, they undergo additional specialised training in interventional procedures. This dual skill set equips interventional radiologists to not only interpret diagnostic images but also perform intricate and precise interventions, contributing to the advancement of patient care through minimally invasive approaches.
Therefore, a foundational training in general radiology is imperative to comprehend the diverse imaging manifestations of various medical conditions. This knowledge serves as a critical foundation for interventional radiologists to make informed decisions and execute procedures in a safe and effective manner, this is essential for the safety of both the patient and the operating team (for eg: radiation risk). In India, interventional radiologists primarily operate within the radiology department. However, as an emerging trend, increasing number of centres globally, and a select few in India, now boast dedicated IR departments akin to other clinical specialties.
What are the different interventional radiology procedures and what systems are covered under IR?
- Neuro-interventions:
- Stroke interventions – mechanical thrombectomy.
- Endovascular aneurysm repair (coil or intrasaccular devices) and AVM embolization,
- Middle meningeal artery embolisation for cSDH,
- Caroticocavernous fistula/Dural arteriovenous fistula (AVF) embolization.
- Cortical venous thrombus thrombolysis, Carotid artery stenting.
- Preoperative embolizations (juvenile nasopharyngeal angiofibroma, meningioma etc)
- Intra Arterial chemoperfusion for brian and ocular tumours (retinoblastoma)
- Endovascular shunt (eShunt) for hydrocephalus.
- Central vascular interventions (except coronary) –
- TEVAR
- Central venous angioplasty in dialysis patients and for SVC syndrome
- IVC filter placement ro prevent PE.
- Aortic interventions –FEVAR/BEVAR, EVAR (Endovascular aortic repair – thoracic/abdominal) and CERAB.
- Iliac stenting.
- Visceral arteries – Celiac, SMA and IMA plasty/stenting
- IVC thrombolysis, plasty, and stenting.
- Peripheral vascular interventions:
- Arterial revascularisation by not only Angioplasty and stenting of limb arteries but also with newer technology – atherectomy, lithotripsy, deep venous arterialisation and percutaneous transmural arterial bypass (PTAB).
- DVT thrombolysis, mechanical thrombectomy.
- Varicose vein ablation – RFA, LASER, microwave ablations and/or foam injection sclerotherapy, glue therapy.
- Vascular malformation – injection sclerotherapy
- Percutaneous Dialysis fistula creation, dialysis salvage interventions like Fistuloplasty, and thrombolysis.
- Chemo Ports, PICC line and other tunnelled insertion.
- Thoracic interventions:
- Bronchial artery embolization for massive hemoptysis.
- Thrombolysis and Mechanical thrombectomy in acute pulmonary embolism.
- Pulmonary AVM embolisation
- Thoracic duct embolisation to manage post surgical complications like chylous leak.
- Bronchial stent placement.
- Ablation of lung lesions.
- Long term, tunnelled pleural drain – eg. PleurX
- Lung biopsy for mass lesions in difficult areas.
- GI and hepatobiliary interventions:
- Embolization of bleeding vessels, either due to trauma or iatrogenic or due to pseudoaneurysms (for eg. post pancreatitis, post surgical or post ERCP sphincterotomy)
- Transjugular intrahepatic portosystemic shunt (TIPSS) in acute variceal haemorrhage or refractory ascites/hepatic hydrothorax in cirrhosis as a bridge to transplant or in Budd-Chiari syndrome.
- Variceal obliteration in uncontrolled variceal haemorrhage – BRTO, P/CARTO etc.
- Portal vein interventions – in portal vein thrombosis
- Percutaneous mesocaval shunt creation for chronic PV occlusion not amenable to recanalisation.
- Percutaneous transhepatic biliary drainage (PTBD) and stenting.
- Endobiliary biopsy and ablation.
- Esophageal, duodenal or colonic stenting, Radiologically inserted percutaneous gastrostomy.
- Transarterial chemoembolization (TACE) or TARE (radioembolization) for hepatocellular carcinoma (HCC),
- Portal vein embolization prior to liver resection to promote compensatory hypertrophy to achieve enough functional reserve before resection.
- Transjugular liver biopsy (TJLB) in severe coagulopathy/ascites,
- Bariatric embolisation – embolisation of left gastric artery.
- Hemorrhoidal artery embolisation.
- Long term, tunnelled peritoneal drain – eg. PeritX
- Genitourinary interventions:
- Renal artery angioplasty for RAS.
- Renal artery embolization for pseudoaneurysms, AVF (traumatic or iatrogenic – often post biopsy or nephrostomy)
- Renal angiomyolipoma embolisation.
- Percutaneous renal denervation for resistant hypertension.
- Percutaneous nephrostomy, ureteric stenting.
- Microwave and radiofrequency (RFA) ablation for RCC.
- Transjugular renal biopsy.
- Prostate artery embolization for BPH.
- Testicular vein embolization for varicoceles
- Uterine artery embolization for postpartum haemorrhage (a real lifesaver! and saves the uterus too).
- Uterine fibroid embolization.
- Fallopian tube recanalization
- Ovarian vein embolization in pelvic congestion syndrome.
- Musculoskeletal interventions:
- Ablation of osteoid osteoma.
- MSK embolisations eg.Geniculate artery embolization for osteoarthritic pain in the knee which prevents or delays knee replacement.
- MSK ablations for soft tissue tumours.
- Vertebroplasty and augmentation.
- Intramedullary nailing for fractures.
- Ozone therapy for disc degenerative disease.
- USG guided intra articular and nerve root steroid injection.
- Foetal interventions
- Foetal blood sampling
- Intrauterine foetal blood transfusion
- Vesico-amniotic shunt for foetal lower urinary tract obstruction
- Amniocentesis/Amnioinfusion
- Chorionic villus sampling
- Interventional pain management:
- Vertebral/sacral/ augmentation in osteoporotic metastatic fractures/ impending collapse
- Thermal ablation of painful metastatic lesions
- Nerve plexus alcohol ablations (neurolysis) in chronic pain, USG guided nerve blocks.
- Interfacetal/transforaminal or epidural steroid injection for chronic back pain.
- Ozone therapy of disc prolapse.
- Percutaneous cervical cordotomy – for severe cancer pain
Phew! That is one exhaustive list indeed!
Almost all systems are covered under interventional radiology. IR offers an image-guided minimally invasive alternative for most of the surgical procedures involving all systems across all specialties. IR plays a pivotal role in modern oncology.
Interventional Radiology – Cases.
Here are a few IR operations to demonstrate the wide variety of cases IR tackles :
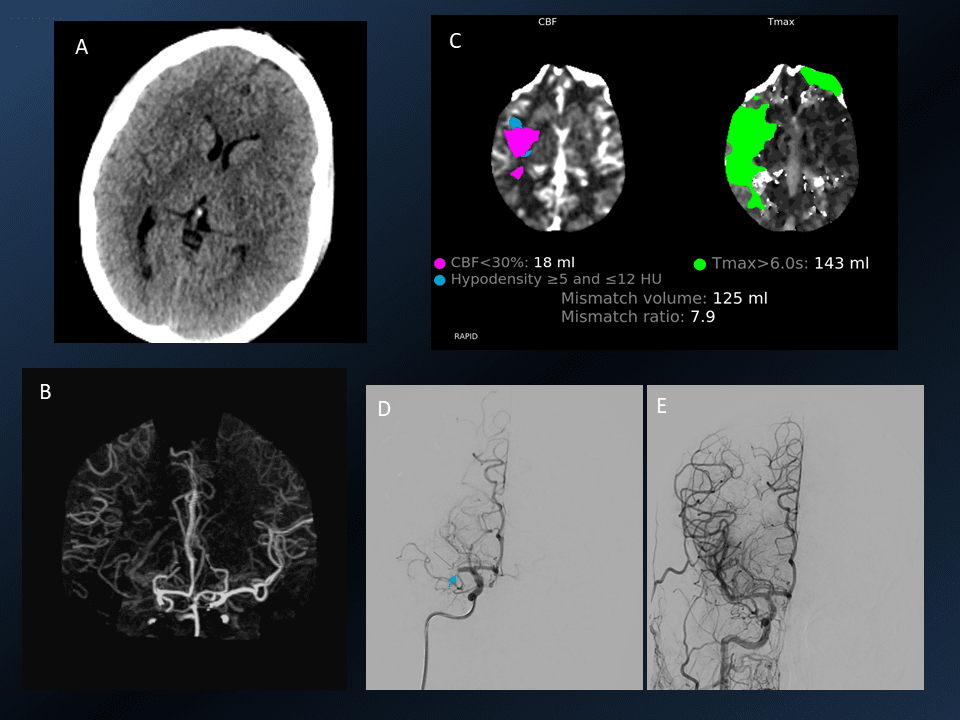
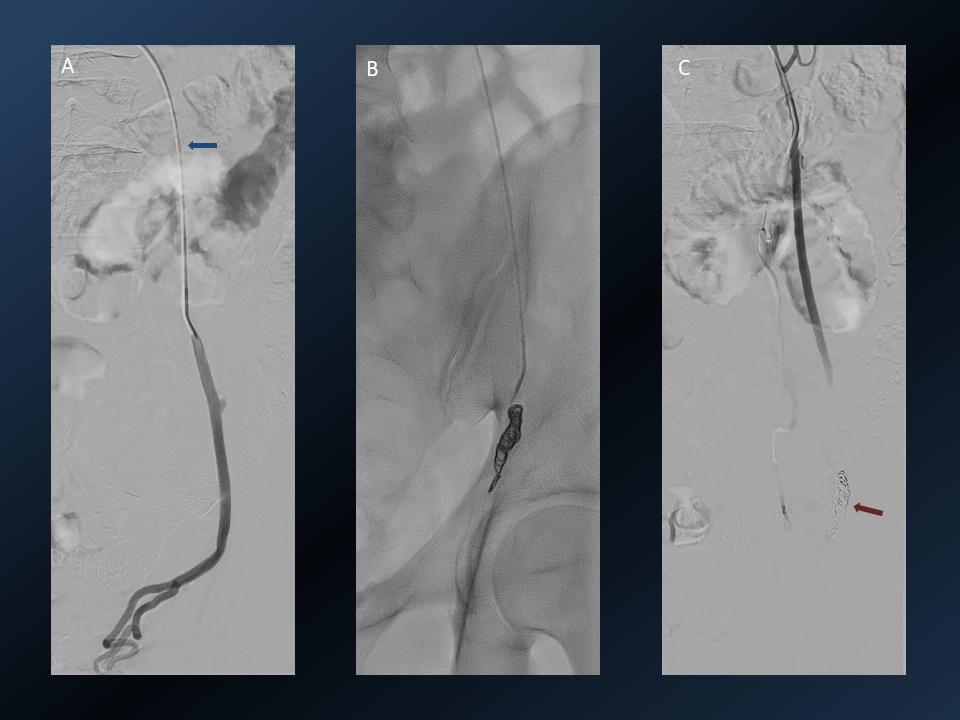
3D rotational images and subsequent angio cine of a successful mechanical thrombectomy of left MCA clot (TICI 3).
1. Mechanical Thrombectomy using stentriever and aspiration technique





The pre and post procedure angiograms are of the above case.
2. Intrasaccular device for intracranial aneurysm embolisation

3. Mechanical Thrombectomy with aspiration only technique
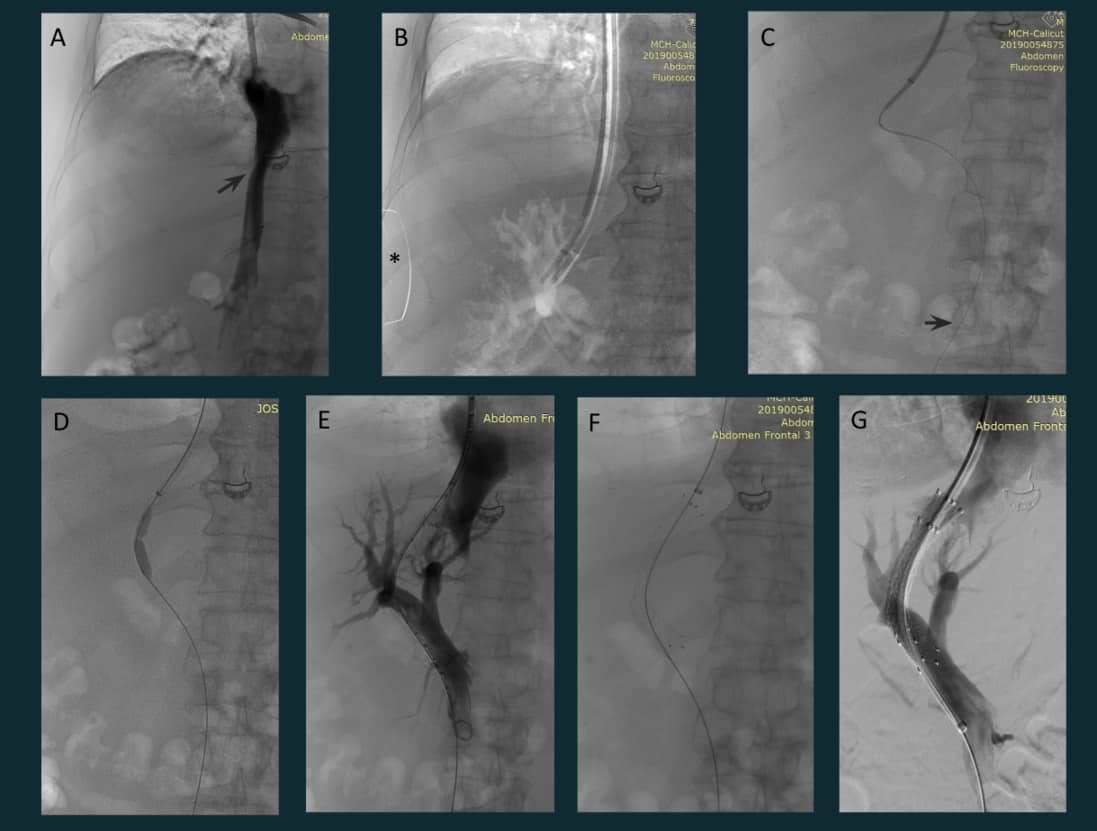
4. TACE (Transarterial Chemoembolization)

4a.TACE (contd)

5. Palliative embolization of bleeding metastatic lesion

6. USG guided embolization of bleeding pseudoaneurysm

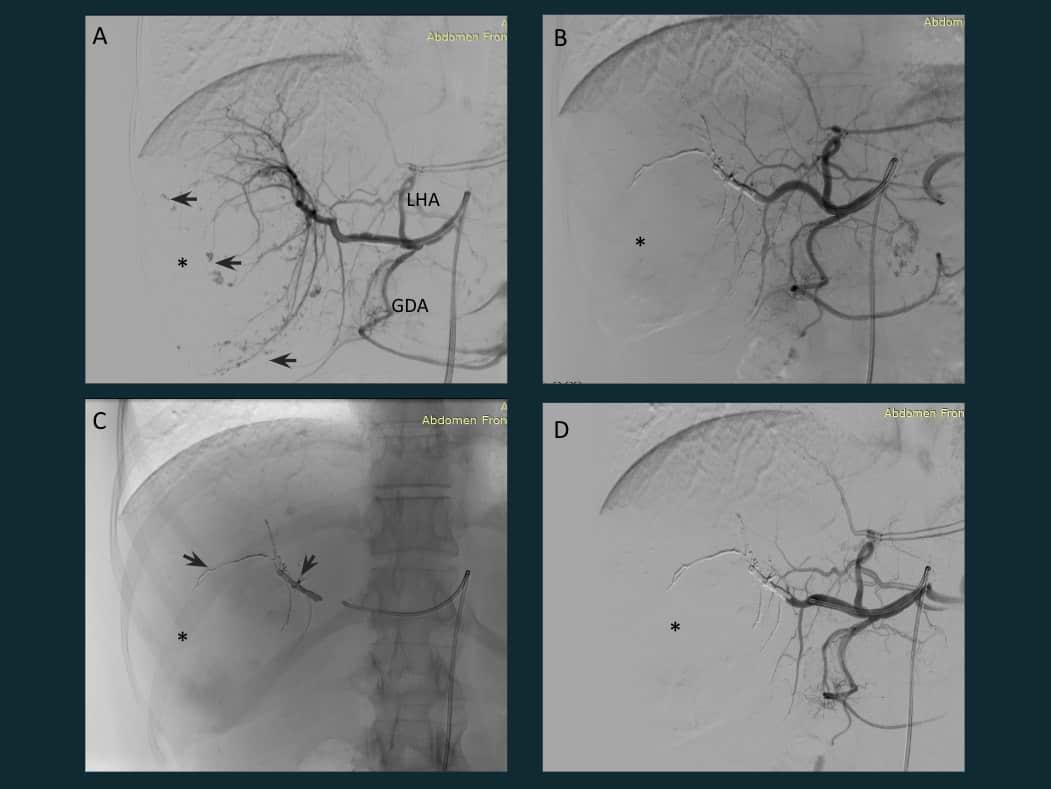
7. Transjugular intrahepatic portosystemic shunt (TIPSS)
8. Giant hepatic hemangioma embolization
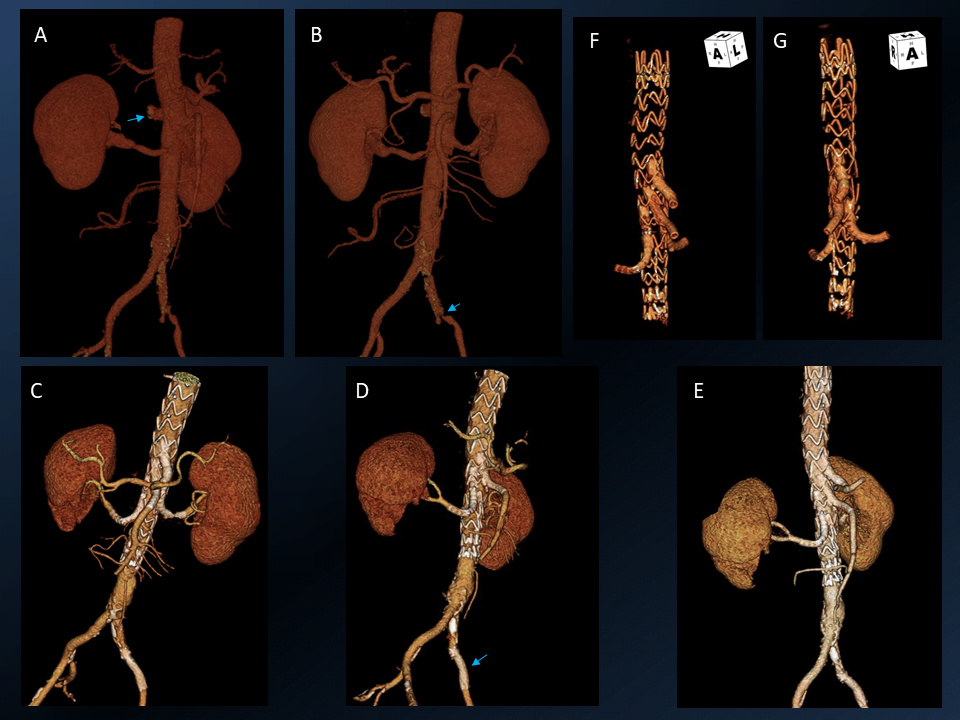
9. EVAR
EVAR stands for Endovascular Aneurysm Repair.
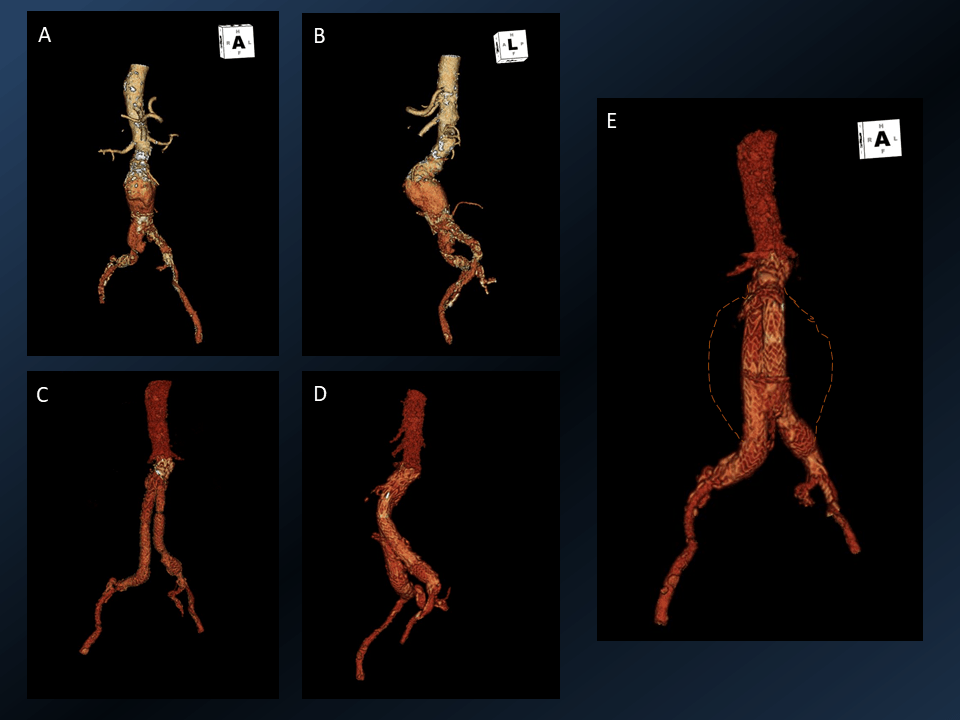
3D reconstructed images of infrarenal abdominal aortic aneurysm (AAA) before (A & B) and after (C, D & E) endovascular aneurysm repair. Imaginary contour of the original aortic wall (orange dotted line).
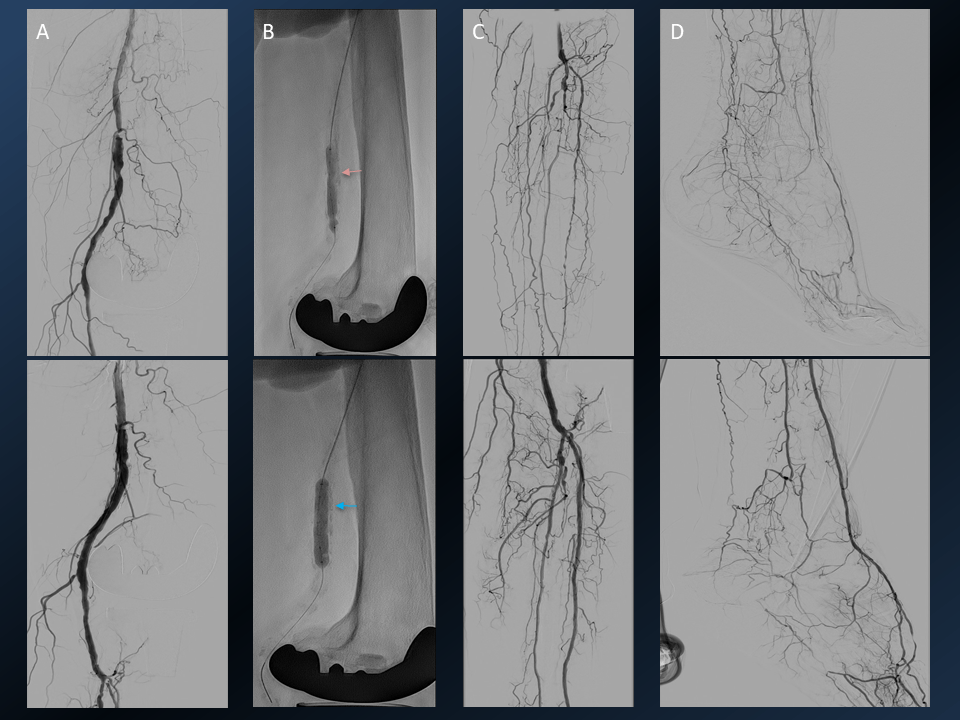
10. BEVAR
BEVAR stands for Branch Endovascular Aneurysm Repair
11. Intravascular Lithotripsy (IVL)
12. Gastrointestinal haemorrhage embolization

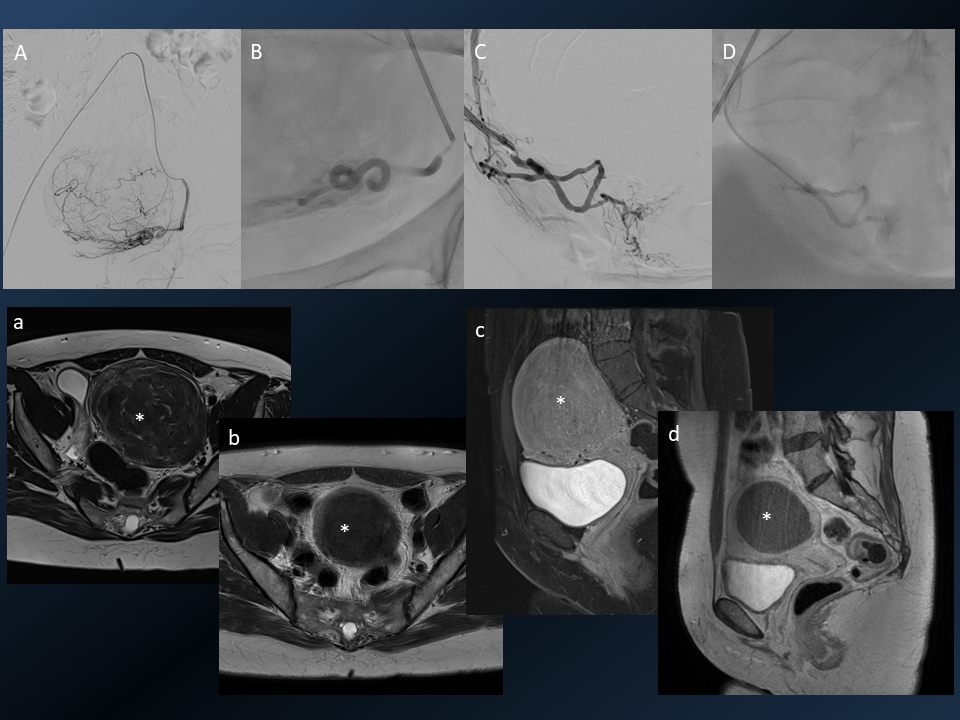
13. Renal Angiomyolipma (AML) Embolisation

14. Uterine fibroid embolization (UFE)
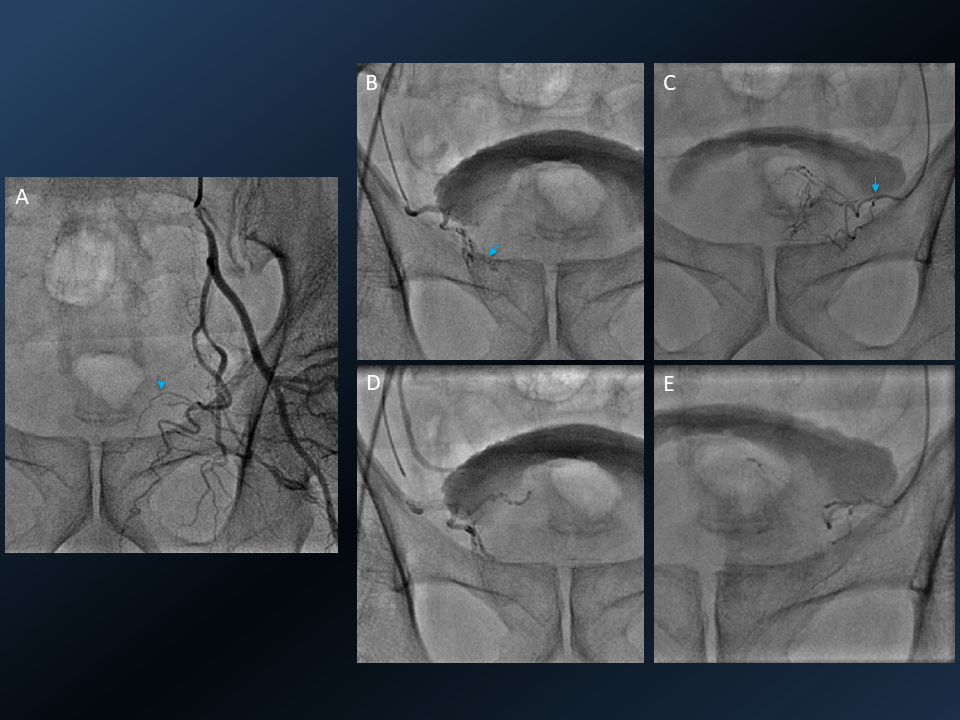
15. Prostate Artery Embolisation (PAE)
16. Varicoele Embolisation
17. Percutaneous Transhepatic Biliary Stenting
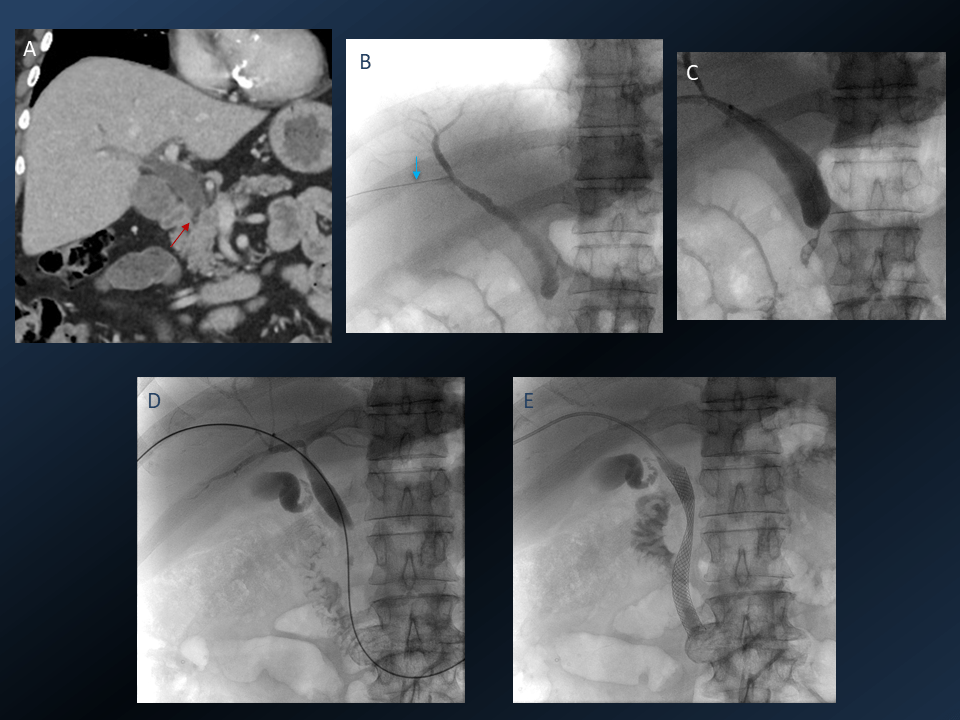
18. Esophageal stent placement

19. Percutaneous Gastrostomy

20. Microwave ablation of Osteoid osteoma

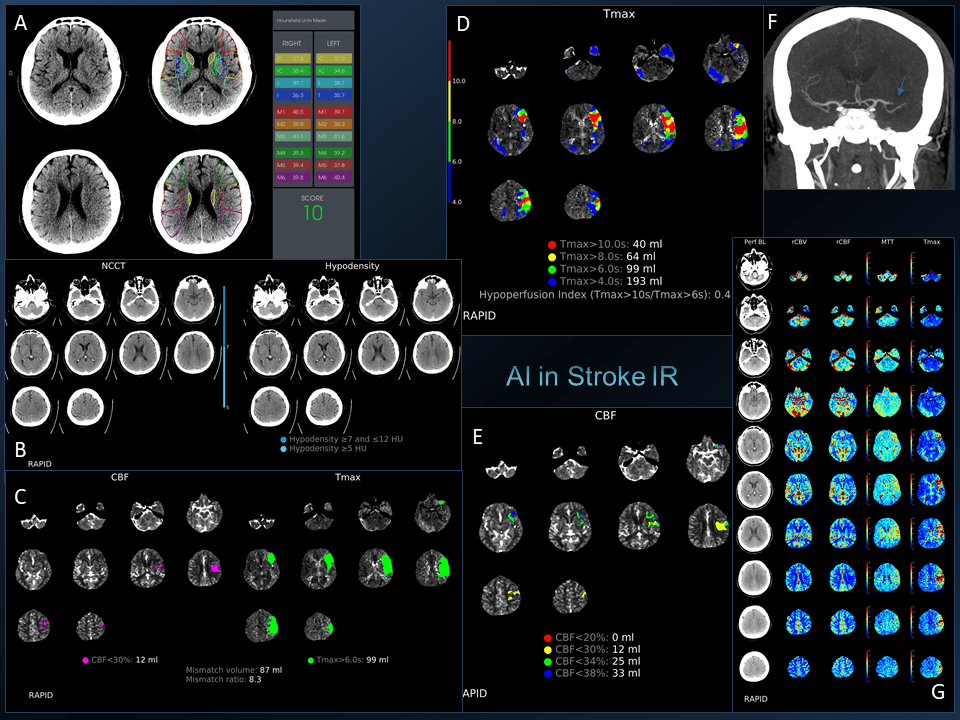
21. Use of AI in Interventional Radiology – Acute Stroke
Check out our post on some Interventional Radiology Instruments:
Spotters Set 35 – Interventional radiology wires and catheters!
Interventional Radiology – Training.
How can I become an Interventional Radiologist?
Easy and tough! Radiology residency is the basic requirement and where the core training happens. IR training can vary from 1-2 year fellowships to 3 year courses. There are 3 – year DM and DNB courses in IR in many institutes. Also, there are DM Neuroradiology and Interventions and DM Cardiothoracic imaging and interventions which usually are focussed to a particular system diluted with diagnostic imaging.
There are initiatives to consider an independent 6 year IR course after MBBS incorporating basic surgical and diagnostic radiology training. In the US, it is already a well sought-after, independent, 6-year postgraduate training program. The UK is also heading towards the same path with IR specialty status in the near future.
The Royal College of Radiologists in the UK has approved a dedicated IR training curriculum recently.
Simply put, the best way is to get trained in a good center with lots of exposure in all aspects of IR and hands-on training. The “degree” really doesn’t matter in terms of hands-on training and wide exposure. Some of us are fortunate to be trained by excellent teachers and to have great mentors both in our home country and abroad (so true, for me it is India and the United Kingdom).
In my opinion, a maximum of two years of training at a reputable high volume centre is sufficient to master most of the “MCA to Dorsalis pedis” IR. Ideally, pursuing two distinct fellowships, each lasting 12-18 months, is valuable, especially for those aspiring to specialise in some newer neurointerventions such as stroke mechanical thrombectomy (EVT). This approach allows individuals to benefit from the expertise of mentors from different institutes, each with unique workloads, rather than an extended duration at a single location.
This perspective holds true for those considering fellowship opportunities abroad as well, given that each centre tends to specialise in particular areas of intervention, be it neuro, aortic, or oncological procedures. While this dual fellowship approach may not be feasible for everyone due to practical constraints, it provides a nuanced and comprehensive training experience, enhancing proficiency across different facets of Interventional Radiology.
Read this detailed post on this topic here:
From Medical School to Residency: The Path to Becoming an Interventional Radiologist
How do I pursue a fellowship in IR?
Most of the hospitals which run an IR fellowship select candidates based on an entrance test (comprising MCQs on general radiology and basic interventions).
Here are some things to look out for:
- Make sure that you join a good center with a good teacher and enough number of cases and an optimal number of junior IRs.
- Beware of those hospitals which conduct fellowships (not only in IR but also in other subspecialties, especially cross-sectional imaging and MSK) just for the sake of getting doctors for cheap labor.
- Make sure that you get a decent stipend.
- Do visit the hospital and the cath lab and get the stats.
- A neat hack is to speak to the cath lab tech or nurse. Often it will give you an accurate idea about the caseload and the work culture than from the current fellows 😉
Where can I pursue an IR fellowship?
Here is a list of institutions that offer an interventional radiology fellowship in India compiled from the Indian Society of Vascular and Interventional Radiology. For more fellowship updates you can check this telegram channel.
How many interventional radiology training seats are there in India?
The number of training opportunities have improved a lot in the last 3 years. At least 50 DM/DNB (3 year) and nearly 100 fellowships (1-2 year) are available in India as of 2024 (at the time of writing this article in 2019 this was around 10 and 64 respectively).
What steps can one take during radiology residency if one intends to pursue IR?
If your institute has an IR division, make full use of the IR rotations. If you show genuine interest most of the IRs are very good teachers and will try to teach you. Attempt to learn how to do US guided venous cannulation, arterial access by the modified Seldinger technique, and if possible perform a few diagnostic angiograms.
You should be familiar with basic image-guided procedures and biopsy techniques like USG guided lymph node, liver and renal biopsy, CT guided lung/vertebral biopsy, USG/CT guided pigtail drainage of collections. Try to understand the basic IR devices like catheters, guidewire, balloons, stents etc.
Practicing IV cannulation in the CT and MR room (with and without US guidance) is a good start and it will be a valuable asset for your practice.
A few specific queries from residents in this context:
I just cleared DMRD and going for secondary DNB and what should be my approach if I want to learn interventional radiology what kind of options are available in India, and how much time it takes to become a practicing interventional radiologist after post-graduation?
Ideally, you should look for a center that has a good IR division. In fact, a Radiology department with a fully equipped IR division is more respected by other specialties as well. Now all the reputed hospitals have an IR division with at least two interventionologists. Start assisting cases and build a good rapport with the IR team. (In case they run a fellowship, this will be an added advantage later). You can join them after your DNB and start assisting them and learn if the consulting IR is a good teacher.
Is there any fellowship of interventional radiology just after DMRD clearance or second DNB is a must?
It is better to do your fellowship after at least 3 years of experience in general radiology. Best is to practice 1-year diagnostic radiology, independently in a high volume center before moving into a dedicated IR training. Most of the centers which offer fellowship expect post DMRD plus one year experience.
Where can I train for varicose veins and other peripheral vascular interventions in India?
Minimally invasive IR treatment for varicose veins is part of the IR curriculum. Most of the centers which offer IR training perform ablative and non-ablative treatments for varicose veins - RFA/LASER/MW ablations, sclerotherapy and glue therapy.
Contrary to US, UK and other European countries where peripheral arterial interventions are already a major workload of IR, in India this took a back seat due to the trade off between vastness of the IR procedures vs shortage of trained IRs (And cardiologists were never in short supply!) However, this is making a rapid comeback as more and more trained IRs perform excellent peripheral arterial interventions nowadays. Few hospitals allow vascular surgeons or cardiologists to perform these procedures purely due to logistics reasons, hence make sure that your IR department is also involved in peripheral vascular work.
Which countries are offering fellowships in IR and what is the pathway to those fellowships?
Countries like Canada, Australia, and the UK offer IR fellowships.
FRCR is required for the UK (recently there is a good number of vacancies that have come up in the UK, maybe due to the Brexit effect). The MTI programme by RCR is an alternative pathway to get UK training before passing FRCR if you have good credentials and prior experience from your home country. Link in reference. Some trusts in the UK offer fellowships post FRCR 2A too.(https://www.jobs.nhs.uk/candidate)
Many universities in Canada and Australia offer IR fellowships, but they are mostly looking for people with prior IR experience (like a fellowship from India). For France and Germany, you can apply if you meet the language requirements.
Check this webpage for IR Fellowship listings in Canada: https://cairweb.ca/en/ir-fellowship-programs-in-canada/
Here is information for IR fellowships in Australia from the RANZR website:
The interventional training journey starts within the RANZCR Clinical Radiology Training Program, where registrars develop a range of basic procedural and clinical competencies. This training program lays the foundations required for interventional practice, which can be built upon through Continuing Professional Development (CPD) activities or by undertaking a Fellowship in IR or INR upon receiving the FRANZCR.
These Fellowship positions equip radiologists to perform complex procedures requiring specialised interventional skills. With hospitals increasingly recognising the value of IR and INR in delivering cost-efficiencies and optimal patient outcomes, radiologists who complete these Fellowships often go on to practice in full time IR or INR consultant positions.
Fellowships for Interventional Radiology are typically one year in duration. Once the Fellowship is completed, some IRs choose to sit the European Board of Interventional Radiology (EBIR) examination, hosted by the Interventional Radiology Society of Australasia (IRSA) at their annual meeting.
Fellowships for Interventional Neuroradiology are a minimum two years in duration. Once the Fellowship is completed, INRs can apply for a recognition of training in INR through the Conjoint Committee for the Recognition of Training in Interventional Neuroradiology (CCINR).Fellowships are offered at most major hospitals and some regional centres. For a list of current Fellowship opportunities, please visit the RANZCR Jobs website.
What are the MCI approved degrees for IR??
MCI approves only MD/DMRD/ DNB/DM degrees. No fellowships in any specialty are recognized by the MCI (currently). In fact, IR is part of postgraduate radiology curriculum and a residency in radiology -MD/DNB/DMRD itself medico-legally qualifies you to perform interventions. However, it is always ethical to perform interventions you are trained in (not that you are confident in your own skills). There is a surge in the number of fellowship courses and radiologists wanting to do advanced IR training recently. Make sure that you join a good center with a good number of cases and enough hands-on experience is provided.
How to prepare for IR super specialty (NEET SS) entrance exam?
Not sure about this. Just like any other entrance exam, your diagnostic radiology must be strong. Get an overall idea about basic IR procedures and some basic knowledge on advanced and latest interventions. You can refer to a few basic IR books.
Totally how many IR seats are available in India?
Approx 150. Please refer to the NEET SS brochure.
What are a few recommended books for IR?
There are many books available. As a resident, it is better to choose one or two books and stick to it. For residents/fellows –Handbook of Interventional Radiologic Procedures by Kandarpa is a good handbook. Here are a few more books for Interventional Radiology :
Here are a few good IR textbooks:
As practicing IRs, we refer to journal articles for the standard protocols and the best practice for a particular procedure. Here are a few good IR journals apart from the (regular diagnostic radiology journals):
- Journal of Vascular and Interventional Radiology (JVIR).
- Cardiovascular and Interventional Radiology (CVIR).
- Seminars in Interventional Radiology.
- Journal of Clinical Interventional Radiology ISVIR
Interventional Radiology - Job.
We plan two days OPD, three days operating and one day for research activities and/or for sorting the cath lab and inventory in a week. But in reality, a busy IR sees patients and references every day, mostly referred from other departments and operates daily too, in addition to the emergency calls.
The IR OPD in tertiary care hospitals are equipped with an US machine. A typical IR consultation involves review of images (CT, MR or radiographs), on site US scan combined with clinical examination. No wonder IRs are otherwise called superhero doctors. No other specialty makes use of technology and skills to this extent.
A typical day is as follows.
8 AM: Day starts with ward/ICU rounds to assess the post-op patients. Then back in the IR cath lab to reassess the patients posted for that day by reviewing the images. Most of the cases are planned on the day of admission itself.
9 AM: We start the cases posted on that day. 1-2 major procedures and 2-3 minor -procedures are done on a normal day. Certain procedures like neuro coiling for aneurysms, Aortic interventions like FEVAR and TIPSS (Transjugular intrahepatic portosystemic shunt) may take most of the day and are usually done under general anesthesia, hence requiring at least 3 hours. Percutaneous EVARs are done under local anaesthesia.
In between the cases, we see the out-patients/referrals. Imaging is of prime importance in addition to clinical examination for decision making. Hence if the ideal imaging modality, which is most of the time essential for pre-procedural planning is not done, the patient is directed to get it done in a day or two and follow up (unless there is an emergency). A quick US scan also may happen depending on the case.
3 PM: We wind up by around 3 PM and there will be a post-op ward round in the evening before we leave the hospital. Also, there are occasional emergency night calls for cases ranging from simple pigtail insertion, percutaneous nephrostomy or biliary drainage to GI or stroke thrombectomy, visceral bleeder embolization (traumatic or pseudoaneurysms), bronchial artery embolization for hemoptysis, postpartum haemorrhage or acute cholangitis.
In centers where there are neuro-interventions, stroke calls for mechanical thrombectomy (MT or EVT) is a routine. This can make your life really unpredictable. But EVT is one of the most rewarding IR procedures which no IR would want to opt out of.
Patients are always curious about the complication rate. How can we explain complication rates to a patient on various CT / USG guided biopsies and drainage procedures etc?
While explaining to patients we need to be more careful. Every procedure, just an IV access, at least theoretically can cause serious complications and can even risk life. The art lies in imparting awareness to the patient without inducing undue fear. Informed Consent is a must like any other surgical procedures and all preprocedural investigations and preparations are to be done without compromise.
In evaluating complication rates, a valuable perspective can be gained by comparing them with traditional surgical procedures, where interventional radiology consistently demonstrates lower rates. Drawing from relevant articles, such as comparisons between splenectomy and splenic artery embolization or hysterectomy and fibroid embolization, allows us to provide patients with informative insights. By juxtaposing the potential outcomes of open or laparoscopic surgeries with minimally invasive, pinhole procedures in interventional radiology, we naturally alleviate patient concerns, facilitating a more informed decision-making process.
How to balance diagnostic radiology and interventions? I have apprehensions that once I pursue interventional radiology, my diagnostic skill will take a backseat.

As an IR you will always evaluate the patient with your clinical and radiologic skills. Obviously, you will be using more of your radiological skills, especially ultrasound since it gives much more information than any clinical examination method.
For instance, a typical IR consultation involves history taking and a brief casual talk, then straight away image review (CT/MRI/PET). Clinical examination for IRs is screening USG (it’s basically a combination of traditional clinical contact with the patient with a USG scan). Most of the time, this will be a game-changer and sometimes a complete twist in the diagnosis is also seen.
In short, as an interventional radiologist, your diagnostic skills will improve, be it in any modality – plain films, USG, CT or MRI, even better than a diagnostician in that particular system. Personally, I have seen IRs having better Doppler skills.
If you are not seeing brain MRIs for a while or not performing breast USG, there will be an initial lag when you re-start doing it, and that’s not insurmountable. A couple refresher courses or some reading can swiftly place you back in the fast track. If you are not used to doing reporting once in a while, your reporting skills, like elaborating a condition, its description, etc might take the back seat – but who really cares as long as your report solves the clinical dilemma.
Ultimately a good diagnosis or advice that helps patient management matters more than a two pages-long report (which nobody reads!) with a suboptimal final impression.
Should I be concerned about the radiation exposure working as an Interventional Radiologist?
Radiation exposure is a significant consideration in interventional radiology. Similar to handling any powerful weapon, here too responsibility and expertise are paramount. The comprehensive understanding of Radiology Physics acquired during training distinguishes interventional radiologists (IRs) from other medical practitioners utilizing radiation equipment. Adherence to established protocols for radiation protection devices and employing basic practices to minimize radiation exposure are essential. While it's crucial to respect the power of radiation, there's no need for undue fear.
In the average IR practice, the dose of radiation exposure is unlikely to pose a health risk, provided one adheres to safe radiation practices. Direct exposure is minimal, except in rare instances such as occasional hand exposure during left-sided PTBD procedures. As the saying in IR goes, a proficient operator's expertise is evident on the screen, not in their hands.
Watch this detailed video on radiation risk:
Radiation Risks – Separating Hype from Substance!
What are the future prospects of IR is smaller and tier 2 cities in India?
In the realm of medical specialties, while Radiology was considered a booming field, Interventional Radiology (IR) stands out as an ever-expanding and dynamic specialty. If diagnostic radiology feels threatened by AI (unlikely to replace radiologists) AI enhances the capabilities of IR (For eg: Use of AI softwares in Stroke, Onco and Aortic interventions). Innovations in the field of IR are coming out almost on a daily basis and that’s the awesomeness of IR. There will be a time when every specialty in medicine will rely on IR (it is already the standard of practice in developed parts of the world). In fact, most of the surgical procedures are becoming obsolete by the advent of safer and effective IR alternatives (eg. Uterine fibroid embolization, Prostate artery embolization for BPH, TIPSS, etc).
There are established IRs, even in tier-II cities. But the problem in developing countries is the resource limit. Most of the hospitals share a cath lab (catheterization lab – nothing to do with “only coronary catheterization”) and it will be under the ‘custody’ of cardiologists’. Hospital managements have started realizing the importance of IR and have started appointing IRs with allotting them an equal share of cath lab time (Of course, to perform advanced procedures like aortic and neuro-interventions we need a better cath lab with advanced DSA machine than the ones used for coronary angioplasty). Previously patients from smaller cities were referred to metro cities like Mumbai, Delhi, and Bangalore or to bigger institutes for IR procedures. Now more reputed hospitals have realized the potential of IR and installed dedicated IR cath labs and patients don't have to travel distances.
Because of this the unethical practice of other specialty doctors like cardiologists and surgeons attending IR cases have drastically reduced for better patient care and safety. This is only going to improve with more hospitals getting IR cath labs and IRs.
What basic interventional procedures does one needs to know during residency and does it matter if we have very limited exposure to IR during residency?
The exposure to Interventional Radiology during residency doesn't necessarily determine your competence. While having exposure is an added advantage, the real benefit is a smoother learning curve if you've had prior experience.
Basic interventions like USG guided FNAC/Bx, pigtail drainages (CT/USG guided) helps you to acquire good coordination and probe orientation skills. Also a bit of patient management. Know about basic drugs like local anaesthetics, analgesics, antibiotics and sedatives and its reversal agents.
How much can I earn as an Interventional Radiologist?
Earnings are like any other surgical specialty. IRs can be seen as one of the top paid doctors in India and US. It also depends on the place that you practise and the kind of work that you do. Initial pay can be similar or slightly higher than that of a diagnostic radiologist. However, once you establish your own practice the earnings will be in the upper strata among doctors.
Is it really worth to opt for intervention radiology now? I got a pessimistic reply from most of the people that you spoke to.
Always ask an IR about IR if you wish to pursue IR.
As it is for any other specialty, doctors who do not practice IR, cannot have a true perspective about the specialty. Half-IR kills the IR trainee (and the patient)! The most important thing is to get into a good center for training where there are good mentors. If you are not sure - Research! Go to the hospital and visit their cath lab.
What is the role of IR technologists?
A good IR tech is an asset to any IR suite.
They can play in a wide variety of roles, from an IR nurse to store manager depending on what the situation demands. Their help is invaluable in every aspect of IR practice not only during the procedures but also in things like procuring and sorting our devices, device selection, preparing the materials like embolization agents and so on. Unlike most of the cardiology cath lab techs, they are trained radiographers. Most of them are people who have worked with other IRs and have good knowledge about different procedures that you might be doing for the first time.
Sometimes they can give you a valuable tip from their previous experience in a difficult situation. I have learned many new things from each and every IR tech that I have worked with.
Is IR a good career option in India and abroad, especially in the Middle East?
Most of the centers in India now realise the need for an IR and are actively recruiting. The absence of an IR in their team is an indirect indicator that the hospital needs much improvement to deliver the current standard of care. Most hospitals look for an economically viable option of hiring a person who can do head to toe interventions. This reiterates the importance of mastering IR as a whole rather than limiting it into a subspecialty and combining it with its corresponding diagnostic radiology subspecialty (for eg: Abdominal imaging and IR). However, bigger centres can afford subspecialist IRs eg. MSK or breast interventions.
There are some places where the general radiologist expects IRs to report their own cases. There is already a trend of a separate division of IR in many big centers. So that IR is treated as a separate referral wing, for example, like General surgery.
The Middle East has many vacancies, but most of these want you to have an experience of at least 2-3 years.
Is IR purely dependent on referral like diagnostic radiology and is there any scope of independent OPD practice?
All IRs now have their own OPDs. Many of them have their own wards too apart from ICU beds. After all, it is teamwork. The entire hospital needs to work as a team and specialties should support each other for everyone's benefit. After all, we exist to work together towards better patient care.
Is the job as an interventional radiologist stressful?
It depends on how you take it.
I find it exciting. You get that adrenaline rush for sure. If you know your limitations and when to stop and what not to take up, it is a fun world full of new devices and innovative procedures. Literally every other day you come across a new procedure. Most importantly many of these procedures are life-saving and replace complex/debilitating surgical procedures.
Trust me, working as an IR - satisfaction is guaranteed!
I am quite bad at procedures. Can I still get good at IR?
Like any other job, this is very subjective and depends on the person's attitude towards the job.
The main disadvantage is ergonomics and radiation risk. In comparison with diagnostic radiology, IRs have to face a lot of ergonomic issues and the stress related to patient management. These can be managed by keeping yourself fit both physically and mentally.
You might be the only IR covering more than one hospital. In this case, you might end up attending emergency cases very often.
Also, you may not get the luxury of "after 5 PM forget work" life. You might get endless calls from the hospital after the day's work, mostly regarding post-op management. Almost like a busy surgeon-life.
Another 'disadvantage' is that often you have to explain and convince clinicians about procedures. Because most of the IR procedures are novel, other clinicians are usually very keen and excited to know about it. Some of them may even want to learn a particular procedure because usually, an expert IR makes things look very easy.Most often, you see yourself talking to the hospital management too, trying to prove that some particular procedure is done worldwide by an Interventional radiologist and not by a cardiologist or a surgeon. Not so rarely, by citing references from reputed journals. Sometimes this can happen even with your diagnostic colleagues who mention in their report: "suggested cardiology opinion regarding further management". This can be frustrating at times. Miseries of practicing a relatively new specialty!
At the end of the day, if you feel it's all worth it, then you will never find these as hardships.
Closing thoughts:
During my training days, a memorable statement from one of my professors in a usual ‘philosophical’ discussion stuck with me: "Think about this – among those aspiring to become doctors, only a fraction actually get the chance/opportunity. Among them, less than 10% secure their preferred postgraduate specialty, and of those, less than 10% venture into Radiology. That's a stroke of luck."
Expanding on this notion, I'd add, "Among these fortunate radiologists, only a select few, a small percentage get into interventional radiology. It truly feels like a blessing, doesn't it?
However, the landscape has evolved, and there are now more training positions, attracting a growing number of individuals aspiring to be IR specialists. IR, with its innovative and surgical-like nature, is an exciting field, but it comes with a vital reminder - the timeless adage:
'With great power comes great responsibility!'"
References and Resources
- von Ende E, Ryan S, Crain MA, Makary MS. Artificial Intelligence, Augmented Reality, and Virtual Reality Advances and Applications in Interventional Radiology. Diagnostics (Basel). 2023 Feb 27;13(5):892. doi: 10.3390/diagnostics13050892. PMID: 36900036; PMCID: PMC10000832.
- Artificial Intelligence and Acute Stroke Imaging. J.E. Soun, D.S. Chow, M. Nagamine, R.S. Takhtawala, C.G. Filippi, W. Yu, P.D. Chang, American Journal of Neuroradiology Jan 2021, 42 (1) 2-11; DOI: 10.3174/ajnr.A6883
- Sebastian B, Rajesh U, Scott PM, Sayeed S, Robinson GJ, Ettles DF, Shrivastava V, Lakshminarayan R. Prophylactic Uterine Artery Embolization in Placenta Accreta Spectrum-An Active Intervention to Reduce Morbidity and Promote Uterine Preservation. J Vasc Interv Radiol. 2023 Nov;34(11):1922-1928. doi: 10.1016/j.jvir.2023.07.020. Epub 2023 Jul 28. PMID: 37517463. https://doi.org/10.1016/j.jvir.2023.07.020
- Fletcher A, Moore KJ, Stensby JD, Hulbert A, Saemi AM, Davis RM, Bhat AP. The Pain Crisis: Interventional Radiology's Role in Pain Management. AJR Am J Roentgenol. 2021 Sep;217(3):676-690. doi: 10.2214/AJR.20.24265. Epub 2020 Sep 23. PMID: 32966117. https://doi.org/10.2214/AJR.20.24265
- https://www.jobs.nhs.uk/candidate/search/results?keyword=Interventional%20radiology%20fellow&skipPhraseSuggester=true&payBand=DOCTOR_OTHER&language=en
- Adam, A., Kenny, L. Interventional Radiology Should Establish Its Own Identity it Should be a Primary Specialty Separate from Diagnostic Radiology. Cardiovasc Intervent Radiol (2024). https://doi.org/10.1007/s00270-023-03643-3.
- Sebastian B, Keshava SN, Lakshminarayan R. The Status of Interventional Radiology as a Specialty among Medical Students in India-Knowledge, Interest, and Exposure. Indian J Radiol Imaging. 2021 Apr;31(2):259-264. doi: 10.1055/s-0041-1733813. Epub 2021 Jul 28. https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0041-1733813
- https://interventionalnews.com/specialty-status-interventional-radiology/#:~:text=An%20IR%20specialty%20would%20result,required%20in%20hospitals%20and%20regions.
- https://www.rcr.ac.uk/exams-training/specialty-training/clinical-radiology-curriculum/interventional-radiology-curriculum/
- Medical Training Initiative RCR https://www.rcr.ac.uk/exams-training/medical-training-initiative-mti/
- Adam, A., Kenny, L. Interventional Radiology Should Establish Its Own Identity It Should be a Primary Specialty Separate from Diagnostic Radiology. Cardiovasc Intervent Radiol (2024). https://doi.org/10.1007/s00270-023-03643-3

Dr. Bibin Sebastian MBBS MD DNB EDiR FRCR EBIR
Consultant Interventional Radiologist
Department of Vascular and Interventional Radiology
Hull Royal Infirmary & Castle Hill Hospital
Hull University Teaching Hospitals NHS Trust
United Kingdom
Dr Sebastian completed his core Radiology and Interventional Radiology training from St John's and BGS Gleneagles, Bangalore, India and a 2-year advanced clinical IR fellowship by Royal College of Radiologists from Hull University Hospital, United Kingdom.
Interests: Aortic and stroke interventions, Ultrasound guided IR, AI in IR, Cardiac imaging, Music and Reading. Dr Sebastian believes that an imminent independent clinical specialty status of IR could unleash its full potential and can make tremendous advancement of modern healthcare. I would like to thank Dr. Sebastian for the efforts and all those who took the time out to take the survey.
I am sure that this solves a lot of queries for young radiologists who want to pursue IR! If you have more questions, feel free to ask them in the comments section. Alternatively, you can write to Dr. Sebastian.
I do not practice as an interventional radiologist but having worked in a hospital with an awesome IR department and from my interactions with fellow interventional radiologists, here are my 2 cents:
- Interventional Radiology has a steep learning curve like any other surgical branch. You have to invest in a few years of your life to master the skills.
- IRs are very good at diagnostic radiology, at times better than their DI colleagues. Probably because they are better aware of the patient-management protocols.
*Image credits: NIH Flickr gallery










Thank u so much very informative
Glad you liked it Nermeen.
-A.
Thank you so much sir. Very informative.
Sir, will you please tell me how to prepare for DM in GI and hepatobiliary and Genitourinary intervention after doing Md Radiology?
Is there any syllabus for neet ss in Dm IR? Which book should I read?
Sir, this was very informative. Can you please elloborate on eligibility requirements and route to Canadian radiology fellowships.
Are the Licentiate of medical council of Canada and Royal college of Physicians of Canada certification required for applying to Canadian fellowships?
Sure Pavan. I shall write a blog post or make a video on the RadioGyan YouTube Channel.