Quiz
Which of the following signs is seen in Xanthogranulomatous Pyelonephritis?
- Moose head sign
- Bear Paw sign
- Anteater nose sign
- Eye of the tiger sign
Click here for the answer
Answer: Bear Paw sign (Read below).
Where do you see the other signs mentioned? Let me know in the comments below.
Pathophysiology
Xanthogranulomatous pyelonephritis (XPGN) is a chronic granulomatous process, induced by recurrent bacterial urinary tract infection, in which the renal parenchyma is ultimately replaced with lipid-laden macrophages. The condition is frequently unilateral and manifests when there is a persistent renal blockage in the renal pelvis caused by a centrally obstructing calculus, an infection or as a consequence of chronic pyelonephritis. The most common organisms responsible are E. coli, Pseudomonas, P. mirabilis, Klebsiella, or Enterococcus faecalis. It can extend into the perinephric soft tissues as well.
Key Imaging Features
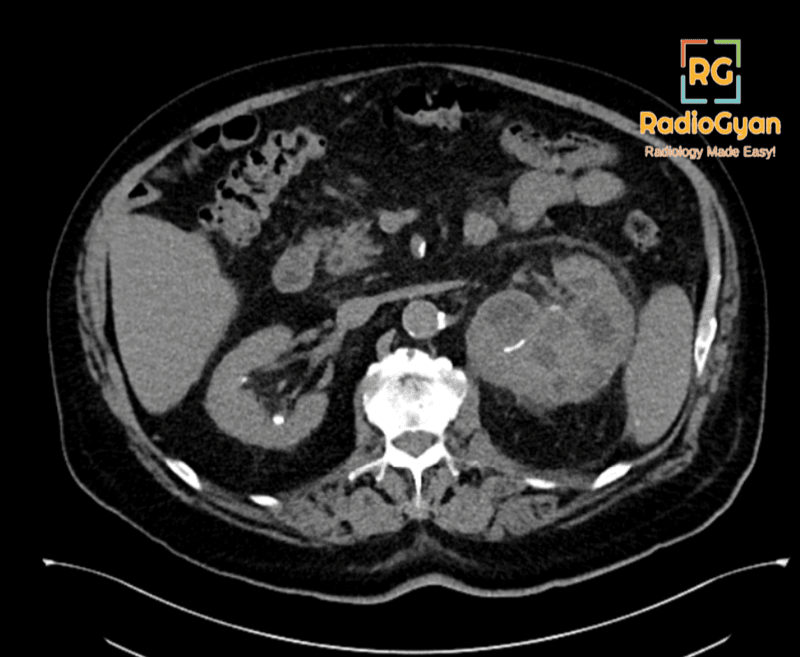
CT–
- Unilateral renal enlargement with preserved reniform shape, signs of extrarenal inflammation and an obstructing renal calculus.
- Non-enhancing, low-attenuation regions seen within the kidneys are dilated renal calyces with pus-filled cavities encircled by compressed, enhancing renal parenchyma giving the appearance of a “bear paw” appearance.
- Although these hypodense areas may simulate fluid and hydronephrosis, these represent low-attenuation inflammatory exudate.
- Decreased renal function characterized by delayed nephrogram and delayed/absent excretion.
USG– distorted and enlarged contour of the kidneys, disintegration of the normal kidney architecture, and typically a central echogenic calculus with shadowing in the renal pelvis (staghorn calculus).
MRI– Iso to hyperintense signal of the solid component on T1-weighted images, compared with the renal parenchyma, depending on the amount of xanthoma cells involved in the granulomatous process, while T2-weighted images show isointense signal, compared with the contralateral normal kidney. The pus-filled cavities appear T1 hypointense and T2 hyperintense. Overall the lesion shows a heterogeneous appearance with solid and cystic components around a core staghorn calculus. Collections will show post-contrast enhancement.
Radiograph and excretory urography– Non-specific findings include an enlarged renal outline, staghorn calculus and reduced renal function on the affected side with no excretion on delayed imaging.
Key Imaging Features:
USG is the first line of investigation however CT scan remains the imaging modality of choice.
Top 3 Differential Diagnosis :
- Renal/perinephric abscess– Renal enlargement, striated or delayed nephrograms, dilatation or effacement of the collecting system with echogenic collecting system debris and fluid-fluid levels within the collecting system. Usually acute presentation as opposed to XPGN which is chronic.
- Renal tuberculosis – Causes papillary necrosis and parenchymal destruction. Imaging features may be similar, however, it is not usually associated with an obstructing staghorn calculus.
- Renal cell carcinoma (RCC)- Enhancing soft tissue density lesion. Usually, XPGN will not show enhancement. Differentiation can be challenging in imaging. Fever and elevated inflammatory markers such as CRP and ESR are seen with XPGN and not with RCC.
Clinical Features
- Fever
- Flank pain
- Macroscopic hematuria
- Weight loss
- Abdominal or lower back palpable mass
- Pyuria, positive urine culture
Risk factors
- Female sex (2:1)
- Middle age (40-60 years)
- Recurrent urinary tract infections and pyelonephritis
- Diabetes Mellitus
- Immunocompromised state
- Renal transplant
Classification systems:
Based on Renal Involvement.
- Diffuse renal involvement
- Focal: Involvement within the cortex of the kidney.
Based on the involvement of adjacent soft tissues.
- Stage I: only renal parenchyma is affected by the disorder.
- Stage II: extends to the perirenal fat and affects renal parenchyma.
- Stage III: the disease has spread to the peri- and para-renal areas or the widespread retroperitoneum.
Etymology and synonyms :
Xantho means yellow in greek, indicating the replacement of renal parenchyma by lipid-laden macrophages giving it a yellow color.
Treatment:
Surgical management involves nephrectomy or, in exceptional cases, partial nephrectomy. Antibiotics are used in all cases. Prognosis is good in most cases.
References:
Single best review article
Craig WD, Wagner BJ, Travis MD. Pyelonephritis: radiologic-pathologic review. Radiographics. 2008;28(1):255-328. doi:10.1148/rg.281075171
Other references
- Dalessandro, L. (2021). Xanthogranulomatous Pyelonephritis: A Clinical Analysis. The Journal for Nurse Practitioners, 17(7), 785-788. https://doi.org/10.1016/j.nurpra.2021.04.017
- Rajesh A, Jakanani G, Mayer N, Mulcahy K. Computed tomography findings in xanthogranulomatous pyelonephritis. J Clin Imaging Sci. 2011;1:45. doi:10.4103/2156-7514.84323
- Verswijvel G, Oyen R, Van Poppel H, Roskams T. Xanthogranulomatous pyelonephritis: MRI findings in the diffuse and the focal type. Eur Radiol. 2000;10(4):586-589. doi:10.1007/s003300050967.
Co-Authors: Dr. Mansi Sarmalkar and Dr. Gauri Parvathy.