How to Measure Prostate Volume
Normal Prostate Volume and PSA (Age Specific)
PSA density cut off used is 0.15.
Prostate Volume and PSA Density Calculator: Evidence-Based Applications in Clinical Practice
Key Takeaways
- PSA density (PSAD) demonstrates superior diagnostic accuracy (AUC 0.78) compared to PSA alone (AUC 0.64, p<0.001) for detecting clinically significant prostate cancer
- PSAD cutoff of 0.15 ng/ml/cc offers optimal sensitivity (65%) and specificity (85%) in the diagnostic gray zone (PSA 4-10 ng/ml)
- Stratification by PSAD can significantly reduce unnecessary biopsies (19.7%) while missing only 6.9% of clinically significant cancers using a threshold of ≤0.07 ng/ml/cc
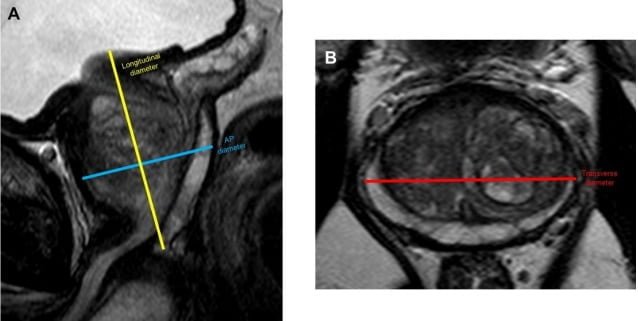
- Prostate volume calculation employs the prolate ellipsoid formula: Volume (cc) = AP × TR × CC × 0.523
- PSAD <0.09 ng/ml/cc indicates minimal risk (4%) of harboring clinically significant prostate cancer (Gleason ≥7) in most patient populations
Clinical Utility of Prostate Volume Assessment
Accurate prostate volume measurement is essential for PSAD calculation and serves as an independent predictive factor in prostate cancer evaluation. Normal prostate volume typically ranges from 25-30cc, with prostatomegaly classified as:
- Mild: 30-50cc
- Moderate: 50-80cc
- Marked: >80cc
The standard volumetric calculation utilizes the prolate ellipsoid formula (V = AP × TR × CC × 0.523), which has demonstrated excellent correlation with pathologic specimens (r=0.89) despite systematic underestimation by approximately 17%. Multiparametric MRI offers superior volume assessment accuracy (ICC 0.91) compared to transrectal ultrasound (ICC 0.71), though TRUS remains the most accessible modality in routine clinical practice.
Normal Prostate Volume (ml) by Age Group and Ethnicity
| Age Group | Caucasian | Japanese | Chinese (Malaysia) | Malay (Malaysia) | Indian (Malaysia) |
|---|---|---|---|---|---|
| 40-49 | 23.5 | 16.8 | 25.5 | 22.3 | 18.7 |
| 50-59 | 30.7 | 17.4 | 24.0 | 25.5 | 26.0 |
| 60-69 | 34.6 | 18.5 | 28.5 | 28.5 | 26.0 |
| 70-79 | 35.4 | 19.1 | 29.1 | 35.0 | 25.3 |
PSA Density: Technical Considerations and Calculation
PSA density represents the normalization of serum PSA concentration to prostate volume. This metric adjusts for the established relationship between gland size and PSA production, addressing a fundamental limitation of PSA testing. The formula is:
PSAD (ng/ml/cc) = Serum PSA (ng/ml) ÷ Prostate Volume (cc)
This calculation has particular relevance for patients with benign prostatic hyperplasia, as larger transition zones naturally produce more PSA. By adjusting for volume, PSAD helps discriminate between benign PSA elevation and potential malignancy, especially in the diagnostic “gray zone” of PSA 4-10 ng/ml.
Normal PSA Density (ng/ml²) by Age Group and Ethnicity
| Age Group | Caucasian | Japanese | Chinese (Malaysia) | Malay (Malaysia) | Indian (Malaysia) |
|---|---|---|---|---|---|
| 40-49 | 0.03 | 0.04 | 0.04 | 0.03 | 0.03 |
| 50-59 | 0.03 | 0.04 | 0.04 | 0.04 | 0.03 |
| 60-69 | 0.05 | 0.05 | 0.05 | 0.04 | 0.04 |
| 70-79 | 0.05 | 0.07 | 0.05 | 0.05 | 0.04 |
Evidence-Based PSAD Thresholds
Multiple studies have investigated optimal PSAD cutoffs, with the following evidence-based thresholds established:
| PSAD (ng/ml/cc) | Clinical Significance | Evidence |
|---|---|---|
| <0.07 | Safe to avoid biopsy | Nordström et al. (19.7% reduction in biopsies, 6.9% missed significant cancers) |
| <0.09 | 4% risk of clinically significant PCa | Aminsharifi et al. (NPV 96% for Gleason ≥7) |
| 0.15 | Standard clinical threshold | Benson et al. (original validation study) |
| 0.19-0.20 | Highest Youden’s index | Catalona et al. (optimal sensitivity/specificity balance) |
For patients with PI-RADS 3 lesions on mpMRI, PSAD assessment offers significant value in biopsy decision-making. Current data suggests PSAD ≥0.15 ng/ml/cc in these patients warrants biopsy consideration, with positive predictive values approaching 60% for clinically significant disease.
Diagnostic Performance Metrics
PSAD consistently outperforms PSA alone across multiple clinical scenarios:
- General detection of clinically significant PCa: PSAD AUC 0.78 vs. PSA AUC 0.64 (p<0.001)
- PSA gray zone (4-10 ng/ml): PSAD sensitivity 65%, specificity 85.2% at 0.155 ng/ml/cc threshold
- PSA >10 ng/ml: PSAD sensitivity 96.6%, specificity 66.7% at 0.175 ng/ml/cc threshold
- Negative MRI findings with elevated PSA: PSAD AUC 0.848 vs. PSA AUC 0.722 (p=0.04)
Importantly, multivariate analyses consistently demonstrate PSAD remains an independent predictor of cancer detection even after adjusting for age, clinical stage, and PSA levels. This independent predictive value highlights PSAD’s significant contribution to clinical risk assessment.
Calculation Methodology
This calculator utilizes the prolate ellipsoid formula for volume calculation followed by the standard PSAD determination:
- Input anteroposterior (AP), transverse (TR), and craniocaudal (CC) prostate dimensions in cm
- Enter serum PSA value in ng/ml
- The calculator computes:
- Prostate Volume (cc) = AP × TR × CC × 0.523
- PSA Density (ng/ml/cc) = PSA ÷ Prostate Volume
For optimal accuracy, prostate measurements should ideally be obtained via multiparametric MRI or transrectal ultrasound performed by experienced operators.
Clinical Applications for Patient Management
PSAD has demonstrated utility across multiple clinical scenarios:
- Biopsy triage: Implementing PSAD thresholds (≤0.07 ng/ml/cc) can reduce unnecessary biopsies by nearly 20% while maintaining high detection rates for clinically significant disease
- Active surveillance candidacy: PSAD <0.15 ng/ml/cc serves as one criterion for active surveillance eligibility in appropriate patients
- Risk stratification with equivocal imaging: For PI-RADS 3 lesions, PSAD significantly enhances predictive accuracy for clinically significant disease
- Post-negative biopsy management: PSAD <0.15 ng/ml/cc after benign biopsy correlates with significantly lower prostate cancer mortality (0.5% vs. 2.0% at 15 years)
Limitations and Considerations
Several methodological considerations should inform PSAD interpretation:
- Volume calculation accuracy varies by modality, with systematic differences between TRUS, MRI, and pathologic specimens
- Racial variations in PSA density thresholds have been reported, with some evidence suggesting lower cutoffs may be appropriate in African American populations
- Medications affecting PSA (5α-reductase inhibitors) require special consideration, with some experts recommending doubling measured PSA values before PSAD calculation
- Substantial prostatitis can elevate PSA disproportionately to volume, potentially inflating PSAD values
Frequently Asked Questions
What is the utility of this Prostate Volume and PSA density Calculator?
You can calculate the volume of the prostate gland using this calculator using values acquired on MRI or Ultrasound. This will give an estimate of the size of the prostate gland. The normal prostate gland is approximately 25-30cc in volume.
Prostate-specific antigen (PSA) is a tumor marker for prostate cancer. PSA density can be used to prognosticate prostate malignancies. Patients with low PSA density can undergo active surveillance while those with higher values may need intervention. As stated by PSA-density might inform biopsy decisions, and spare some men from the morbidity associated with a prostate biopsy and diagnosis of low-grade prostate cancer.
What formulas are used for calculating prostate volume, and what are the cut-off values?
Prostate Volume = (Anteroposterior (AP) length x Transverse (TR) length x Craniocaudal Length )*0.523
Note that the PIRADS 2.1 ACR white paper recommends that the AP and TR length should be measured on the sagittal plane as shown in the image above.
A gland volume of more than 30cc is considered prostatomegaly.
A rough grading system for prostatomegaly is :
30-50cc: Mild Prostatomegaly
50-80cc : Moderate Prostatomegaly
>80cc: Marked Prostatomegaly.
What formulas are used for calculating PSA density, and what are the cut-off values?
PSA density = PSA value/Prostate Volume
Although the cut-off values vary, most papers suggest a cut-off value of 0.15-0.20 above which there is a high chance of the patient having clinically significant prostate cancer.
A recent study states the following optimal cut-off values of PSA density to diagnose clinically significant prostate cancer :
- 0.10 ng/ml2 in biopsy naïve patients i.e. patients who have not had a prostate biopsy
- 0.15 ng/ml2 in patients with a previous negative biopsy.
Sasaki et. al suggested in their study: “To avoid unnecessary biopsies, the PSA density cutoff value of 0.18 would be recommendable for determining a prostate biopsy for Japanese males with a serum total PSA level of 4.1-10.0 ng/ml.”
What are the common causes of prostatomegaly (prostate gland enlargement)?
- Benign prostatic hyperplasia (BPH) – Most common cause of prostatomegaly in elderly men. This causes urinary symptoms due to indentation on the posterior bladder wall.
- Prostate cancer
- Prostatitis
- Prostatic abscess
Should we use PSA or PSA density to prognosticate prostate cancers?
PSA density is preferred over PSA alone as the latter can be elevated in inflammation and in a larger gland.
As per a study by Bruno et. al: “At multivariable analysis adjusting for age, biopsy history, DRE and prostate volume, PSA density emerged as a strong predictor of clinically significant prostate cancer (csPCA) but was not associated with prostatic inflammation. The optimal cutoffs of PSA density to diagnose csPCa and rule out the presence of prostatic inflammation in patients with an elevated PSA (>4 ng/ml) were 0.10 ng/ml2 in biopsy naïve patients and 0.15 ng/ml2 in patients with a previous negative biopsy. PSA density rather than PSA should be used to evaluate patients at risk of prostate cancer who may need additional testing or prostate biopsy. This readily available parameter can potentially identify men who do not have PCa but have an elevated PSA secondary to benign conditions.”
In another study, Sasaki et.al conclude: “PSA density was significantly more accurate than other variables in predicting PCa. To avoid unnecessary biopsies, the PSA density cutoff value of 0.18 would be recommendable for determining a biopsy for Japanese males with a serum total PSA level of 4.1-10.0 ng/ml.”
What is clinically significant prostate cancer (csPCA)?
Clinically significant cancer is usually defined as a Gleason Score of more than or equal to 7 on biopsy.
References
- Stephan C, et al. The ratio of prostate-specific antigen (PSA) to prostate volume (PSA density) as a parameter to improve the detection of prostate carcinoma in PSA values in the range of < 4 ng/mL. Cancer. 2005;104(5):993-1003.
- Aminsharifi A, et al. The use of prostate specific antigen density to predict clinically significant prostate cancer. Sci Rep. 2020;10(1):20015.
- Nordström T, et al. Prostate-specific antigen (PSA) density in the diagnostic algorithm of prostate cancer. Prostate Cancer Prostatic Dis. 2018;21(1):57-63.
- Catalona WJ, et al. Comparison of prostate specific antigen concentration versus prostate specific antigen density in the early detection of prostate cancer: receiver operating characteristic curves. J Urol. 1994;152(6 Pt 1):2031-2036.
- Benson MC, et al. The use of prostate specific antigen density to enhance the predictive value of intermediate levels of serum prostate specific antigen. J Urol. 1992;147(3 Pt 2):817-821.
- Karvonen J, et al. Association of prostate-specific antigen density with prostate cancer mortality after a benign result on systematic transrectal ultrasound-guided prostate biopsy. BJU Int. 2023;131(1):72-80.
- Murtuza A, et al. Evaluating the Diagnostic Accuracy of MRI-Derived Prostate-Specific Antigen (PSA) Density in Prostate Cancer Detection and its Association With Tumor Aggressiveness. Cureus. 2022;14(1):e21981.
- Price AK, et al. Determination of Prostate Volume: A Comparison of Contemporary Methods. Acad Radiol. 2019;26(10):1382-1390.
- Ng CW, Lim J, Liu X, Cheng C, Hong GE, Teo J, et al. Ethnicity Is an Independent Determinant of Age-Specific PSA Level. PLoS One. 2014 Aug 11;9(8):e104917.
Check out more radiology calculators :
Frequently Asked Questions Regarding Prostate Volume and PSA Density Calculations
Disclaimer: The author makes no claims of the accuracy of the information contained herein; this information is for educational purposes only and is not a substitute for clinical judgment.
References:
- Bruno, Salvatore, et al. “PSA Density Help to Identify Patients With Elevated PSA Due to Prostate Cancer Rather Than Intraprostatic Inflammation: A Prospective Single Center Study.” Frontiers in Oncology, vol. 11, 2021, https://doi.org/10.3389/fonc.2021.693684. Accessed 17 Dec. 2022.
- Sasaki R, Habuchi T, Sato K, et al. The clinical utility of measuring total PSA, PSA density, gamma-seminoprotein and gamma-seminoprotein/total PSA in prostate cancer prediction. Jpn J Clin Oncol. 2000;30(8):337-342. doi:10.1093/jjco/hyd089.
- Nordström T, Akre O, Aly M, Grönberg H, Eklund M. Prostate-specific antigen (PSA) density in the diagnostic algorithm of prostate cancer. Prostate Cancer Prostatic Dis. 2018;21(1):57-63. doi:10.1038/s41391-017-0024-7
- Lim J, Bhoo-Pathy N, Sothilingam S, et al. Ethnicity is an independent determinant of age-specific PSA
- Flevel: findings from a multiethnic Asian setting. PLoS One. 2014;9(8):e104917. Published 2014 Aug 11. doi:10.1371/journal.pone.0104917


About the Author
Dr. Amar Udare, MD, DNB
Dr. Udare holds an MBBS and MD degree, and his expertise lies in the field of radiology. He has authored multiple peer-reviewed publications, contributing significantly to the medical field. His works can be accessed on PubMed and Google Scholar.
In addition to his academic and professional achievements, Dr. Udare is an avid reader and enjoys exploring the latest advancements in medical technology. His commitment to making complex medical knowledge accessible to patients and the general public aligns with our mission at RadioGyan.com.
For any further questions or clarifications, feel free to reach out to Dr. Udare via the contact form.