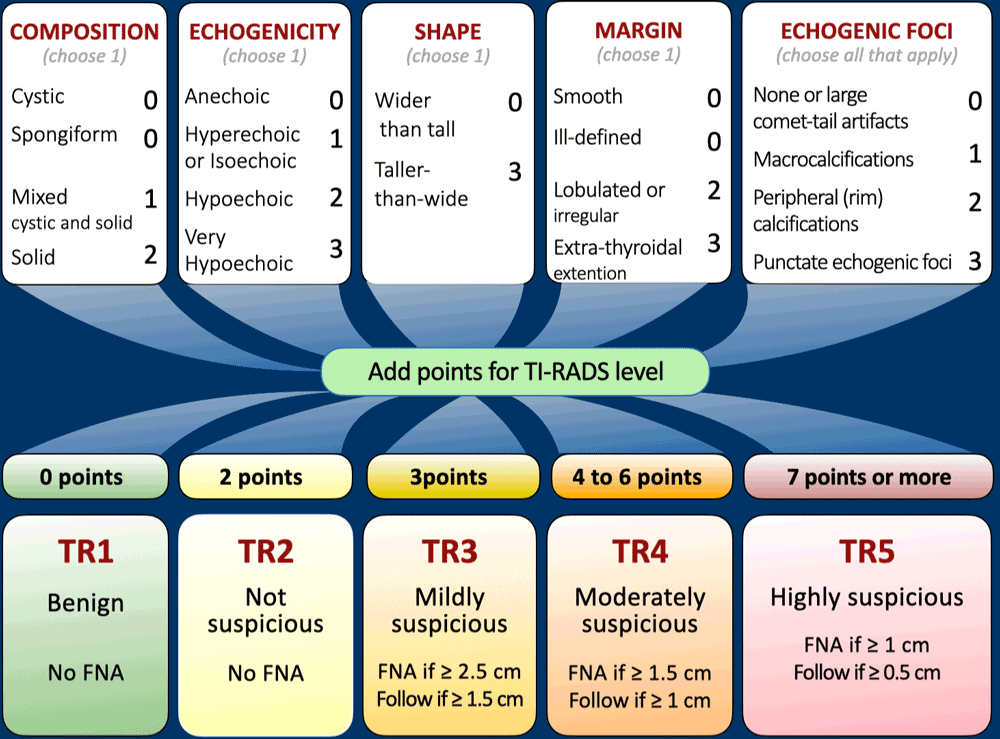
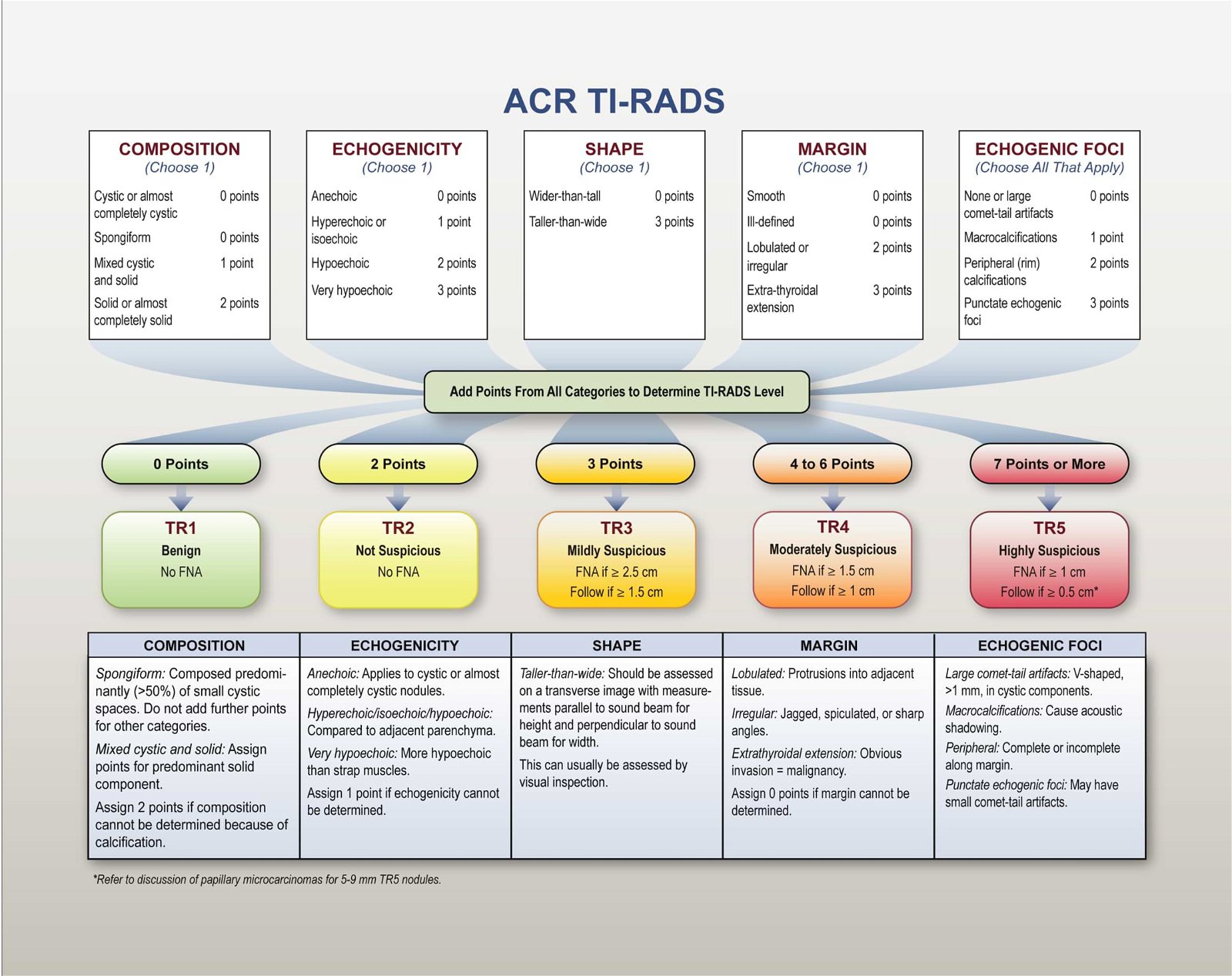
TIRADS Classification Table
|
| Category |
Points |
Suspicion |
Risk of Malignancy |
Guideline |
| TR1 |
0 |
Benign |
0.3% |
No FNA |
| TR2 |
2 |
Not suspicious |
1.5% |
No FNA |
| TR3 |
3 |
Mildly suspicious |
4.8% |
If ≥2.5 cm: FNA If ≥1.5 cm:Follow up at 1,3 ,5 years
|
| TR4 |
4-6 |
Moderately suspicious |
9.1% |
If ≥1.5cm: FNA If ≥1 cm:Follow up at 1,3 ,5 years
|
| TR5 |
7 or more |
Highly suspicious |
35% |
If ≥1 cm: FNA If ≥0.5 cm follow annually for 5 years
|
FNA- Fine Needle Aspiration.
Risk of Thyroid Malignancy depending on TIRADS score
- TR 1 thyroid nodules have a 0.3 % risk of malignancy.
- TR 2 thyroid nodules have a 1.5 % risk of malignancy.
- TR 3 thyroid nodules have a 4.8 % risk of malignancy.
- TR 4 thyroid nodules have a 9.1 % risk of malignancy.
- TR 5 thyroid nodules have a 35 % risk of malignancy.
Caveats for Thyroid Ultrasound Calculator
- If rim calcifications obscure the nodule completely, choose composition to be “solid” and echogenicity to be “isoechoic”.
- If the margin cannot be determined, choose “ill-defined margin”.
- If echogenicity cannot be determined, choose “isoechoic”.
- If composition cannot be determined, choose “solid”.
- Punctate echogenic foci and taller-than-wide features have the highest points so carefully evaluate these.
Key points from the original TIRADS article:
Composition
Cystic or almost completely cystic nodules are generally benign, as are spongiform nodules predominantly composed of small cystic spaces. Solid components with suspicious characteristics may warrant further evaluation for malignancy.
Echogenicity
Echogenicity evaluation involves comparing a nodule’s reflectivity to adjacent thyroid tissue, except for very hypoechoic nodules where strap muscles serve as a reference point. Special consideration is given to anechoic nodules.
Shape
A taller-than-wide shape, when assessed in the axial plane by comparing height and width measurements, can be highly specific for malignancy.
Margin
Ill-defined or irregular margins, especially with protrusions or lobulations, should raise suspicion. Extension beyond the thyroid border should also be considered.
Echogenic Foci
Different types of echogenic foci carry varying levels of suspicion. Punctate echogenic foci within solid components are particularly concerning and should be evaluated in conjunction with other features.
Papillary Thyroid Microcarcinomas
Biopsy of nodules smaller than 1 cm is generally not recommended; however, exceptions may be made based on specific circumstances. Guidelines recommend against routine biopsy of such small nodules unless actively surveilling, ablating, or considering lobectomy for papillary microcarcinomas.
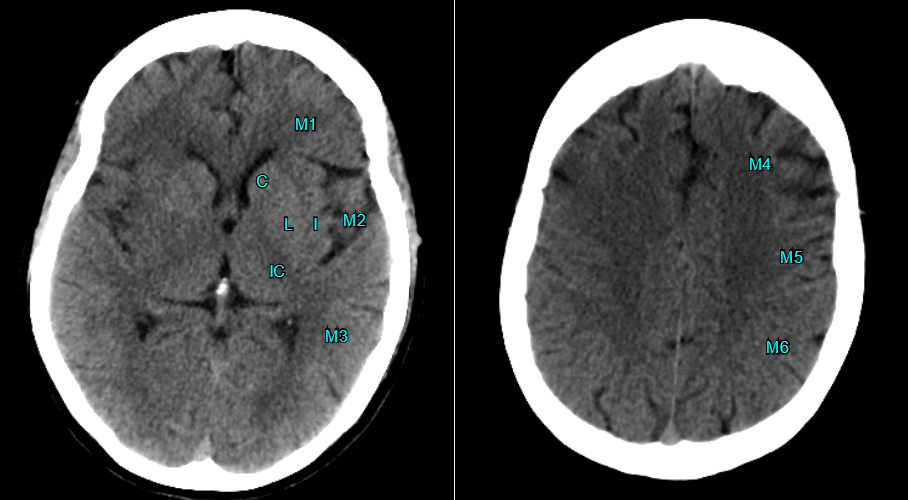
Measurement and Documentation
Accurate sizing and detailed documentation of nodule location are crucial for monitoring and comparison over time.
Definition of Growth
Significant enlargement is defined as a 20% increase in at least two nodule dimensions with a minimal increase of 2 mm or a 50% or greater increase in volume.
Timing of Follow-Up Sonograms
- Optimal spacing for follow-up sonograms for nodules not meeting FNA size criteria lacks consensus in the literature.
- Scanning intervals of less than 1 year are generally not recommended, except for proven cancers under active surveillance.
- Follow-up intervals should be based on the nodule’s ACR TI-RADS level, with more suspicious lesions requiring additional sonograms.
- For TR5 lesions, annual scans for up to 5 years are recommended.
- For TR4 lesions, scans at 1, 2, 3, and 5 years are advised.
- TR3 lesions may undergo follow-up imaging at 1, 3, and 5 years.
-
Imaging can be discontinued at 5 years if there is no size change, indicative of a benign behavior.
- Management of nodules enlarging significantly but remaining below FNA size threshold at 5 years lacks published guidance, but continued follow-up is likely required.
- If a nodule’s ACR TI-RADS level increases on follow-up, the next sonogram should be scheduled in 1 year regardless of its initial level.
Number of Nodules to Biopsy
Biopsy of two nodules with the highest suspicious appearance is recommended to avoid unnecessary procedures and patient discomfort.
Assessment of Cervical Lymph Nodes
Specific features indicating metastasis should prompt FNA of suspicious nodes along with up to two nodules meeting biopsy criteria based on the ACR TI-RADS guidelines.
TI-RADS FAQ
What does TI-RADS stand for?
TI-RADS stands for Thyroid Imaging Reporting and Data System. It standardizes ultrasound reporting and management of thyroid nodules using a point-based system from the American College of Radiology (ACR).
How do I use the TI-RADS calculator?
1) Perform a complete thyroid ultrasound. 2) Select features for composition, echogenicity, shape, margin, and echogenic foci. 3) Review the total points and TI-RADS category. 4) Follow size-based recommendations for follow-up or FNA.
What are the TI-RADS categories?
TR1 Benign, TR2 Not Suspicious, TR3 Mildly Suspicious, TR4 Moderately Suspicious, TR5 Highly Suspicious. Category is determined by total points assigned to sonographic features.
Which ultrasound features are evaluated?
Five domains: composition, echogenicity, shape (transverse), margin, and echogenic foci. Each domain contributes points that sum to a TI-RADS category.
When should FNA be performed?
Typical ACR size thresholds: TR3 consider FNA ≥2.5 cm; TR4 consider FNA ≥1.5 cm; TR5 recommend FNA ≥1.0 cm. Always apply clinical judgment.
What are follow-up intervals?
Common approach: TR1–TR2 no routine follow-up; TR3: US at ~12 months; TR4: US at 6–12 months; TR5: US at 3–6 months if not biopsied. Modify by size and risk.
How accurate is TI-RADS?
ACR TI-RADS is validated and widely used, improving consistency and reducing unnecessary biopsies. Accuracy depends on image quality and correct feature selection; it does not replace clinical judgment.
Which features suggest benignity?
Spongiform composition, anechoic/cystic nodules, hyperechoic/isoechoic echogenicity, wider-than-tall shape, smooth margins, and large comet-tail artifacts in cystic components.
Which features increase suspicion?
Very hypoechoic echogenicity, solid composition, taller-than-wide shape, irregular/lobulated margins, punctate echogenic foci, peripheral/macrocalcifications, and extrathyroidal extension.
What are TI-RADS limitations?
Ultrasound-only system; interobserver variability; does not directly include clinical risk factors or growth rate; less reliable with diffuse disease. Use alongside clinical context.
Is this tool based on ACR guidelines?
Yes, scoring aligns with ACR TI-RADS white papers and lexicon. The tool is educational and not officially endorsed by ACR.
How to apply TI-RADS in multinodular thyroid?
Score each nodule individually. FNA at a time for no more than two nodules with highest point scores; follow no more than four highest-scoring nodules.
Does nodule size affect management?
Size does not change the TI-RADS score but drives management thresholds for FNA and follow-up. Larger nodules within higher categories warrant earlier action.
Who developed this calculator?
This TI-RADS calculator was developed and is maintained by Dr. Amar Udare, MD, DNB, a board-certified radiologist and Clinical Associate Professor in Diagnostic Imaging (Radiology) at the University of Calgary.
Ultrasound Thyroid Score Explained
For a more detailed guide with examples, refer to the dedicated article here:
TIRADS ACR : What radiologists need to know!
More Resources




About the Author
Dr. Amar Udare, MD, DNB
Dr. Udare holds an MBBS and MD degree, and his expertise lies in the field of radiology. He has authored multiple peer-reviewed publications, contributing significantly to the medical field. His works can be accessed on PubMed and Google Scholar.
In addition to his academic and professional achievements, Dr. Udare is an avid reader and enjoys exploring the latest advancements in medical technology. His commitment to making complex medical knowledge accessible to patients and the general public aligns with our mission at RadioGyan.com.
For any further questions or clarifications, feel free to reach out to Dr. Udare via the contact form.